13 Amazing Facts About Difference Between Unstable Angina and Myocardial Infarction
Unstable Angina and Myocardial Infarction
Unstable Angina and Myocardial Infarction involve chest pain as a symptom, but while unstable angina is usually transient and reversible, myocardial infarction indicates irreversible heart muscle damage.
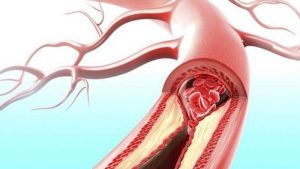
Unstable angina (unpredictable chest discomfort occurring at rest or with minimal exertion due to partial coronary artery blockage), can often be reversed with timely intervention, while Myocardial Infarction (heart attack). On the other hand, involves prolonged coronary artery obstruction leading to irreparable heart muscle damage from complete blockage of one or more coronary arteries causing irreversible muscle damage.
Although both conditions present with chest pain. MI often has radiating and severe discomfort with other symptoms present ECG, biomarkers, and meds are helpful tools in differentiating between them so Unstable angina and MI require lifestyle modifications while MI requires immediate reperfusion therapy or surgery in order to avoid complications like arrhythmias from occurring.
Unstable Angina
Unstable angina is a cardiometabolic condition characterized by episodes of chest discomfort or pain that come on suddenly and unexpectedly – even at rest or with minimal physical exertion. Stable angina tends to be caused by physical activity and tends to follow a regular schedule; in contrast, unstable angina doesn’t follow such a predictable timeline.
Angina is often caused by partial blockages of coronary arteries, restricting blood flow and oxygen supply to the heart muscle. While any discomfort experienced may be transient, it should still be taken seriously as an impending heart attack could be imminent. Individuals experiencing unstable angina might describe its pain as pressure, squeezing, or burning sensation in their chest; shortness of breath; nausea or sweating could all be present as indicators that instability exists.
Unstable angina is a serious indicator that the heart isn’t receiving sufficient oxygen-rich blood. Prompt medical attention must be sought to avoid myocardial infarction (heart attack). Electrocardiograms (ECGs), stress tests, and cardiac enzyme levels help diagnose unstable angina from other conditions medications to manage symptoms and address root causes as well as lifestyle modifications can reduce risk factors and mitigate progression to myocardial infarction (heart attack).
Unstable angina can quickly escalate into something much more serious so understanding its symptoms as well as seeking professional assistance are both vital steps in maintaining cardiovascular health.
Myocardial Infarction
Myocardial infarction, more commonly referred to as a heart attack, occurs when there is prolonged and complete blockage of one or more coronary arteries, restricting blood flow and oxygen supply to parts of the heart muscle, leading to irreparable tissue death and irreversible damage.
A myocardial infarction usually presents with intense chest pain that radiates to arms, jaws, and back unlike unstable angina pain which often feels crushing or pressure-like compared to myocardial infarction’s severe discomfort.
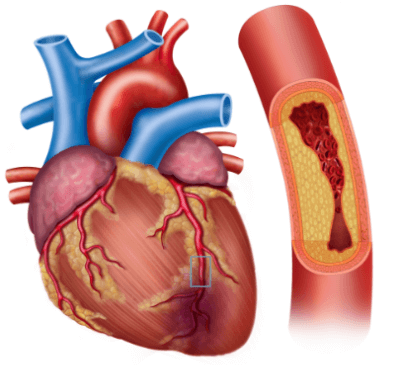
Prompt medical intervention during a heart attack is vital in order to restore blood flow and limit its damage. Emergency reperfusion therapies like angioplasty or thrombolytic medication aim at opening blocked arteries back up again so as to resume blood circulation cardiac enzyme tests and electrocardiograms (ECGs) can be used as diagnostic tools as well as an extensive review of clinical symptoms and medical history in order to accurately diagnose myocardial infarction.
Myocardial infarction survivors can face increased risks of complications, including heart failure, arrhythmias, and sudden cardiac arrest. Lifestyle changes including adopting a heart-healthy diet, regular exercise routine, and medication adherence become integral in reducing further cardiac events.
Recognizing signs of heart attacks quickly seeking medical advice as soon as possible as well as adopting preventive measures are key components to managing myocardial infarctions effectively and improving cardiovascular well-being.
Diagnosis and Medical Assessment
Diagnostic and medical assessments are critical in distinguishing between unstable angina and myocardial infarction (heart attack) as well as determining an effective course of treatment.
Diagnostic and Medical Assessment Services:
Medical History and Risk Factors: Evaluation of Patient Medical History and Risk Factors: Evaluated are past heart conditions, family history, smoking, diabetes and hypertension risk factors such as for example
Physical Examination: A thorough physical exam should include assessments of vital signs such as blood pressure, heart rate and respiratory rate to provide insight into a patient’s cardiovascular health. Examination results can also provide indications as to potential issues within their cardiovascular system.
Electrocardiogram (ECG/EKG): An ECG records the electrical activity of your heart. Changes in its pattern can indicate either low oxygen levels, or actual heart damage; such indicators can help diagnose myocardial infarction more accurately.
Cardiac Biomarkers: Blood tests analyzing troponin levels may provide valuable clues as to heart muscle damage caused by myocardial infarction. An increase in troponin levels indicates muscle tissue injury which often precedes this condition.
Imaging Techniques: Imaging techniques such as coronary catheterization can provide visuals of coronary arteries to identify blockages or narrowing, while echocardiography assesses heart function and any structural abnormalities.
Stress Tests: Stress tests assess how the heart responds to physical exertion, frequently showing decreased blood flow that could indicate unstable angina.
Coronary Angiography: This noninvasive procedure uses contrast dye injected into coronary arteries to visually identify any blockages or narrowing in order to assist treatment decisions and guide treatment strategies.
Clinical Symptoms: Patient-reported symptoms, such as the nature, duration and intensity of chest pain can assist in distinguishing between unstable angina and myocardial infarction.
Differential Diagnosis: Medical professionals consider other potential conditions that could mimic cardiac symptoms, such as gastrointestinal illness and muscle discomfort, which should all be carefully assessed before making their final determinations.
Timely Intervention: For effective management of myocardial infarction, early assessment and intervention – such as thrombolytic therapy or angioplasty – are of utmost importance.
What is the treatment approach for Angina and Myocardial Infarction
Unstable angina and myocardial infarction (heart attack) treatments strive to alleviate symptoms, prevent complications, and promote cardiovascular wellness.
Unstable Angina Treatment: The goal of unstable angina treatment should be to decrease both the frequency and intensity of episodes while also preventing its progression into a heart attack. Lifestyle modifications play a key role, such as adopting a heart-healthy diet, participating in regular physical activity such as cardio, quitting smoking, and managing stress effectively.
Medication may also be prescribed to manage symptoms and increase blood flow – such as Nitroglycerin to dilate blood vessels for reduced chest pain; beta blockers to slow heart rate and blood pressure combination antiplatelet agents such as aspirin prevent blood clots from forming statins to manage cholesterol levels and reduce risks related to plaque build-up.
Myocardial Infarction Treatment: Emergency reperfusion therapies such as angioplasty (using stents to open blocked coronary arteries) and thrombolytics (clot-busting drugs), aim to restore blood flow and minimize damage during a heart attack. Aspirin, antiplatelets, and anticoagulants prevent further clot formation while pain relievers provide temporary relief.
Longer-term management typically involves lifestyle modifications similar to unstable angina and medications. Cardiac rehabilitation programs help patients recover and adopt healthier habits as they work towards recovery and adopt healthier lifestyle changes while cardiac rehabilitation programs help patients adopt healthier habits while recovering.
Effective treatment for both conditions requires taking into account each patient’s health, medical history and risk factors. Early intervention coupled with ongoing medical care and adherence to prescribed therapies plays a pivotal role in improving outcomes and avoiding future cardiac events.
Prognosis and Complications
Prognosis and complications following unstable angina and myocardial infarction (heart attack) are essential considerations in cardiovascular care. Unstable angina left untreated can quickly lead to heart attacks with proper management the prognosis for unstable angina may be positive. Individuals living with unstable angina remain at increased risk of other heart conditions, including heart attacks and heart failure.
Myocardial infarctions are devastating medical events with life-altering implications, with survivors at increased risk for developing heart failure – where the heart struggles to pump blood effectively or arrhythmias, irregular heart rhythms that disrupt normal cardiac function, as well as cardiogenic shock (an inadequate supply of blood to organs). Long-term consequences necessitate significant lifestyle changes, ongoing medical monitoring, and adherence to prescribed treatments so as to mitigate risks and promote cardiovascular well-being.
Comparison chart between Unstable Angina and Myocardial Infarction
Here’s a comparison chart between Unstable Angina and Myocardial Infarction:
| Aspect | Unstable Angina | Myocardial Infarction (Heart Attack) |
|---|---|---|
| Definition | Chest discomfort, unpredictable, at rest/exertion | Prolonged chest pain, severe, crushing |
| Coronary Artery Blockage | Partial blockage | Complete blockage |
| Blood Flow | Reduced, temporary | Severely reduced or absent |
| Tissue Damage | Reversible with prompt intervention | Irreversible, leads to heart muscle death |
| Duration of Symptoms | Brief episodes, relieved by rest or medication | Prolonged symptoms, not relieved by rest |
| Pain Characteristics | Discomfort, pressure, heaviness | Intense, crushing, pressure-like |
| ECG Findings | May show changes during episodes | Distinct ECG changes (ST-segment elevation) |
| Cardiac Enzymes | May be normal during episodes | Elevated cardiac enzymes (troponin) |
| Complications | Risk of progressing to heart attack | Risk of heart failure, arrhythmias, shock |
| Immediate Treatment | Rest and medication | Emergency reperfusion therapy (angioplasty) |
| Diagnosis | Based on symptoms, ECG, cardiac enzymes | ECG, cardiac enzymes, clinical presentation |
| Pain Radiation | Usually localized in chest | May radiate to arm, jaw, back |
| Prognosis | Generally favorable with prompt care | Requires urgent medical intervention |
How do you prevent Strategies of Unstable Angina and Myocardial Infarction?
Preventing unstable angina and myocardial infarction (heart attack) requires both lifestyle changes and medical interventions, which will work together.
Here are strategies to combat each condition:
Preventative Strategies for Unstable Angina:
- Diet for Health: Switch up your eating habits with fresh produce, whole grains, lean proteins and healthy fats while cutting back on sodium-laden processed food and sweets.
- Maintain a Healthy Weight: Through Physical Activity: Engaging in regular physical activity will help to achieve weight management, increase cardiovascular fitness, and decrease blood pressure.
- Tobacco Cessation: Giving up smoking will greatly decrease your exposure to secondhand smoke and may help lower the risk of cardiovascular issues, like atherosclerosis and cardiac issues.
- Stress Management: Utilize techniques such as meditation, yoga and deep breathing to reduce the impact of chronic stress on heart health.
- Medication Compliance: Follow your healthcare provider’s directions when taking medication prescribed to manage risk factors like high blood pressure or cholesterol levels.
- Schedule Regular Medical Check-ups: Conduct routine check-ups with your primary care doctor to monitor blood pressure, cholesterol levels and cardiovascular health. Early detection provides for timely interventions.
Prevention Strategies for Myocardial Infarction:
- Adopt a Heart-Healthy Lifestyle: Adopting a diet rich in whole grains, engaging in regular physical activity, avoiding smoking and managing stress are all ways of living a heart-healthy life that collectively decrease the risk of heart attack.
- Blood Pressure Management: Effective blood pressure control requires dietary modifications, exercise regimens, and taking medicine as directed by healthcare providers.
- Cholesterol Management: Maintain healthy cholesterol levels through diet, exercise, and medications prescribed to lower them if necessary.
- Diabetes Management: If you are living with diabetes, be mindful to maintain optimal blood sugar levels as unchecked diabetes increases heart attack risk.
- Medication: To minimize risk factors and lower the likelihood of a heart attack, consult your physician regarding taking medications such as aspirin, beta-blockers or statins to manage risk factors and lower likelihood of an event.
- Weight Management: To prevent obesity from increasing the risk of cardiovascular disease, balance eating with physical activity to maintain a healthy weight through balanced eating and regular physical activity. Obesity greatly increases heart disease risk.
- Emergency Response Knowledge: To be prepared in case of a heart attack, learn the signs and symptoms and seek medical treatment immediately if they appear.
Final thoughts
Preventing unstable angina and myocardial infarction requires adopting a heart-healthy lifestyle. For unstable angina patients, maintaining a nutritious diet, engaging in regular physical activity quitting smoking as well as managing stress effectively are crucial components.
Adherence to prescribed medication and attending regular check-ups are crucial in the early detection and intervention of myocardial infarction, including controlling blood pressure and cholesterol levels, managing diabetes if present, and leading a healthy lifestyle.
To minimize myocardial infarction risks it’s also crucial that blood pressure, cholesterol levels, and any diabetes-related issues be properly managed, with regular follow-up. Aspirin and statin medications may assist with managing risk factors for heart attacks recognizing their symptoms quickly is also crucial, along with seeking prompt medical assistance for both conditions.
A proactive approach, emphasizing preventative strategies while working closely with healthcare providers for personalized treatment plans may prove more successful in managing both conditions than passive approaches alone.