Difference Between Mycosis Fungoides and Sezary Syndrome
Introduction of Mycosis Fungoides and Sezary Syndrome
Mycosis Fungoides and Sezary Syndrome are rare forms of cutaneous T-cell lymphomas (CTCLs). MF typically affects skin conditions like rashes, plaques, and tumors that progress slowly over time.
In contrast, SS is an aggressive CTCL that involves both skin and blood as symptoms with generalized redness and severe itchy areas resulting from blood tests for diagnosis; staging systems differ between diseases thus impacting treatment decisions and prognosis significantly.
Early detection and accurate diagnosis are essential to effective management. Thus emphasizing their importance for effective management by early detection and accurate diagnosis as early detection and accurate diagnosis are crucially essential.
What is Mycosis Fungoides?
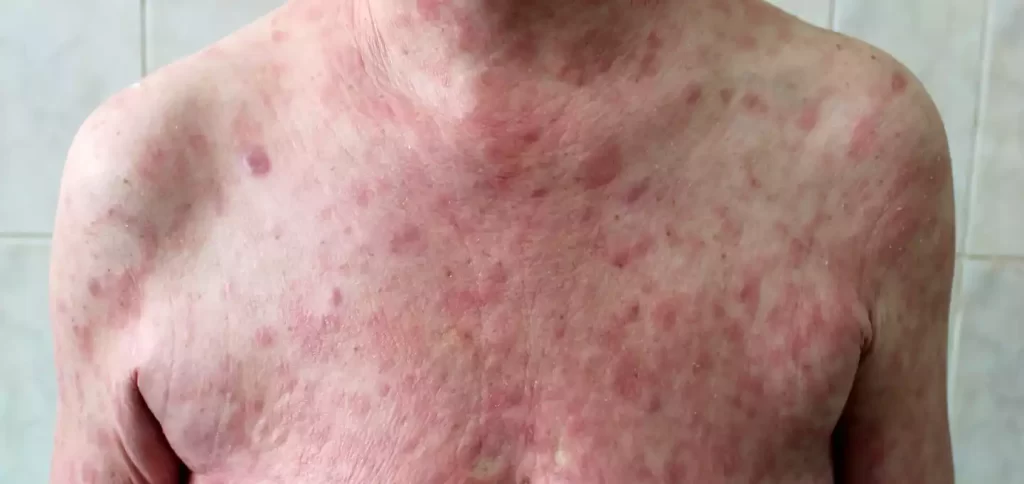
Mycosis fungoides (MF) is an extremely rare non-Hodgkin’s lymphoma form known as cutaneous T-cell lymphoma (CTCL) that predominantly impacts the skin. MF is typically presented as a slow-growing, chronic skin condition characterized by rashes, scaly patches, plaques, and occasionally tumors.
Early stages of MF can often mimic other skin disorders, making diagnosis challenging. Over time, this condition may progress through various stages and affect larger areas of the skin.
Diagnosing Melanoma of the Skin (MF) typically relies on skin biopsies, histopathological examination, and immunohistochemistry analysis. Additionally, using the TNMB staging system – T stands for tumor, N stands for nodes, M for metastases, and B for blood involvement – classification can be made.
Treatment options depend on the stage and severity of the disease and could include topical treatments, phototherapy, radiation therapy, and systemic therapies. While prognosis varies greatly among those diagnosed with MF, early diagnosis and appropriate therapy can improve outcomes significantly.
What is Sezary Syndrome?
Mycosis fungoides (MF) is an extremely rare non-Hodgkin’s lymphoma form known as cutaneous T-cell lymphoma (CTCL) that predominantly impacts the skin. MF is typically presented as a slow-growing, chronic skin condition characterized by rashes, scaly patches, plaques, and occasionally tumors.

Early stages of MF can often mimic other skin disorders, making diagnosis challenging. Over time, however, this condition may progress through various stages and affect larger areas of the skin. Diagnosing Melanoma of the Skin (MF) typically relies on skin biopsies, histopathological examination, and immunohistochemistry analysis.
Additionally, using the TNMB staging system T stands for tumor, N stands for nodes, M for metastases, and B for blood involvement – classification can be made. Treatment options depend on the stage and severity of the disease and could include topical treatments, phototherapy, radiation therapy, and systemic therapies.
While prognosis varies greatly among those diagnosed with MF, early diagnosis and appropriate therapy can improve outcomes significantly.
Signs and Symptoms of Mycosis Fungoides and Sezary Syndrome
Mycosis Fungicides :
- Skin Changes: Microflora typically begins as mild skin symptoms, such as persistent and scaly red patches (erythematous macules) that resemble other conditions like eczema.
- Plaques: As the disease advances, patches can eventually transform into thicker and raised plaques.
- Tumors: Tumors or nodules can develop on the skin in certain instances, potentially becoming cancerous growths.
- Pruritus (itching): It is an all-too-common symptom and can have serious repercussions, impacting quality of life for sufferers.
- Skin Discoloration: Instances of skin discoloration may become either darker or lighter than surrounding tissue, and may alter its tone over time.
- Ulceration: Ulceration and skin breakdown may develop in more advanced cases.
- Unwanted Lymph Nodes: As time progresses, local lymph nodes may swell over time. This could happen as part of their natural enlargement process.
Sezary Syndrome:
- Generalized Erythroderma: Systemic Sclerosis (SS) typically presents as widespread redness (erythroderma) of the skin covering large parts of the body, often covering an extensive surface area.
- Severe Itching: Pruritus in SS may be debilitating and often more intense than with MF.
- Exfoliative Dermatitis: When exfoliation becomes excessive and exfoliation becomes uncontrollable, leading to peeling or shedding of the skin, exfoliative Dermatitis may arise.
- Sezary Cells: In SS, abnormal T-cells known as Sezary cells can be detected in the bloodstream using blood tests.
- Lymphadenopathy: Lymph nodes that swell are a common sign of lymphadenopathy and may become tender to touch.
- Hair Loss: Social Stress can contribute to hair loss on both the scalp and other parts of the body.
- Nail Changes: Alterations in nail thickness or pitting may occur over time.
What is the cause of Mycosis Fungoides and Sezary Syndrome
Mycosis Fungoides:
- Genetic Predisposition Certain genetic changes and mutations could result in an increased chance of developing MF , certain genes haven’t been completely determined.
- Immunological Factors The dysregulation in the immune system especially T-cells is believed to play a major part in the pathogenesis of MF.
- Environmental Factors The exposure to specific environmental substances, including radiation, chemicals or infectious agents has been proposed as possible triggers, though the evidence isn’t conclusive.
Sezary Syndrome:
- T-cell Abnormalities SS is characterized by the increased number of abnormal T-cells, particularly T-cells with CD4+, which are believed to play a role in the progression and growth in the course of disease.
- Immunological Dysfunction As with MF alterations in the immune system which include the dysfunction of T-cells play an important role in the development of SS.
- Genetic and environmental factors: Although specific genetic or environmental triggers haven’t been determined, some studies suggest that genetic predisposition as well as environmental exposures could contribute to the formation of SS.
Key Difference Between Mycosis Fungoides and Sezary Syndrome
Here’s a simplified comparison chart between Mycosis Fungoides (MF) and Sezary Syndrome (SS) to highlight their key differences:
| Characteristic | Mycosis Fungoides (MF) | Sezary Syndrome (SS) |
|---|---|---|
| Classification | CTCL (Cutaneous T-cell Lymphoma) | CTCL (Cutaneous T-cell Lymphoma) |
| Skin Involvement | Predominantly skin | Skin and blood |
| Clinical Presentation | Rashes, plaques, tumors | Widespread redness, severe itchiness |
| Blood Involvement | Typically not involved | Involves atypical T-cells (Sezary cells) in the bloodstream |
| Diagnostic Methods | Skin biopsies, histopathology, immunohistochemistry | Blood tests, skin biopsies |
| Staging System | TNMB (T: Tumor, N: Nodes, M: Metastasis, B: Blood) | TNMB (T: Tumor, N: Nodes, M: Metastasis, B: Blood) |
| Treatment Options | Varied, including topical, phototherapy, radiation therapy, systemic therapies | Aggressive treatments often required, such as photopheresis, chemotherapy, targeted drugs |
| Prognosis | Generally better prognosis | Generally poorer prognosis |
| Importance of Early Detection | Early diagnosis can lead to better outcomes | Early detection is crucial for improved prognosis |
How Are Mycosis Fungoides and Sézary Syndrome Diagnosed?
Mycosis Fungoides (MF):
- Diagnostic Evaluation of Clinical Signs: The initial step typically requires a thorough physical exam by a dermatologist, or healthcare practitioner. They’ll look at the skin of the patient, and look for signs that are typical of MF, like plaques, red patches or tumors.
- skin biopsy: For confirmation of the diagnosis A skin biopsy is conducted. In a skin biopsy, an insignificant portion of the skin is removed and sent to an expert pathologist for evaluation. This procedure helps to determine the abnormal T-cell infiltration which is typical of MF.
- Histopathology and Immunohistochemistry: The skin biopsy is examined under a microscope, and immunohistochemical stains are used to determine the presence of atypical T-cells. This helps distinguish the MF condition from other skin disorders.
- Classification and Staging: When the diagnosis is confirmed, the doctor will determine the stage of the illness by using the TNMB classification system. T is the amount of skin involvement N refers in lymph node involvement M to metastasis and B refers to blood involvement.
Sezary Syndrome (SS):
- clinical evaluation: An extensive physical examination is conducted, with a focus on the identification of widespread erythroderma that is extremely itchy, as well as other signs typical of SS.
- Testing for Blood: A complete blood count (CBC) is conducted to determine if there are any abnormalities, for example, an elevated number of blood-borne white cells. Furthermore, flow cytometry could be used to detect the presence of T-cells that are atypical also known as Sezary cells in the bloodstream.
- The Skin Biopsy Similar to MF the skin biopsy is typically done to determine the presence of T-cells that are abnormal within the skin.
- Classification and Staging: SS is staged by using exactly the same TNMB classification system that is used for MF, with particular importance placed on the amount the involvement of blood (B Stage).
- Additional Tests: Additional tests may be performed to determine the severity of lymph node and skin involvement as well as to rule out any other illnesses.
How do you treat Mycosis Fungoides and Sezary Syndrome?
Mycosis Fungoides (MF):
- Topical treatments: In the early stage, skin-directed treatments are commonly utilized. These include topical steroids and topical chemotherapy agents such as nitrogen mustard as well as topical retinoids.
- Phototherapy treatments using UV light, like PUVA (psoralen along with UVA) and narrowband UVB, are efficient in treating MF lesions on the skin.
- Treatment for Radiation: Radiation therapy that is localized is used to treat particular MF lesions or address larger regions of the affected skin.
- Systemic Therapy: In more severe or aggressive instances, systemic therapies could be required. They can include targeted therapies, chemotherapy, and immunomodulatory medications. Bexarotene (an alcohol-like retinoid) along mogamulizumab (a monoclonal antibody) are two examples of systemic treatments.
- Stem Cell Transplantation In extreme cases or when all other treatments have not worked stem cell transplantation could be considered.
Sezary Syndrome (SS):
- Photopheresis Extracorporeal Photopheresis (ECP) can be a typical method of treating SS. It involves removing blood from the patient, then exposing it to UV light, and then returning it back to the patient. ECP helps decrease the amount of Sezary cells present in the blood.
- Systemic Therapy: Different systemic therapies are utilized for SS such as therapy with a targeted approach and immunomodulatory medications. Alemtuzumab Denileukin Diftitox mogamulizumab and denileukin diftitox are treatments that focus on Sezary cells.
- Allogeneic Stem Cell Transplantation: In severe or resistant cases an allogeneic stem-cell transplant could be thought of. It is the process of replacing the bone marrow cells of a patient with stem cells from a healthy donor.
- Supportive Care The relief of symptoms by using emollients to treat skin care and antihistamines to treat itching may improve the patient’s overall quality of life.
Summary
Mycosis fungoides (MF) and Sezary Syndrome (SS) are two forms of T-cell lymphomas that differ significantly in terms of symptoms and treatments. While both typically affect skin conditions such as rashes or plaques, MF primarily impacts only skin biopsies while blood tests can detect both.
Staging systems and treatment approaches vary between both conditions – usually, Mycosis Fungoides has a better prognosis compared with Sezary Syndrome early detection can improve patient outcomes significantly.
Both diseases must be accurately distinguished in order to provide care that maximizes patient outcomes and optimizes patient outcomes.