What is the Difference Between Syphilis and HIV
Sexually transmitted infections (STIs) are infections transmitted through sexual activity, including vaginal, anal, or oral sex. These can result from bugs, viruses parasites, or fungi. Common STIs include chlamydia, gonorrhea, syphilis, HIV/AIDS, herpes, and HPV.
Many STIs can be asymptomatic, making regular testing crucial. Prevention involves safe sexual practices, including condom use, vaccination (where available), and communication about sexual health with partners. Early detection and treatment are essential to prevent complications and further transmission. Education and awareness play a key role in reducing the prevalence and impact of STIs on public health.
What is Syphilis?
Syphilis is a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum. It can also be transmitted from mother to child during childbirth or pregnancy. Syphilis has various stages, each characterized by distinct clinical manifestations.
The stages of syphilis are as follows:
- Primary Syphilis:
-
- Characterized by the appearance of a painless sore or ulcer, known as a chancre, at the site of infection (typically genitals, anus, or mouth).
- The chancre is highly contagious, and the bacteria can be easily transmitted through sexual contact.
- Secondary Syphilis:
-
- Occurs a few weeks after the appearance of the chancre.
- Symptoms may include skin rashes, mucous membrane lesions, and flu-like symptoms such as fever and fatigue.
- This stage can last for several weeks or months.
- Latent Syphilis:
-
- If left untreated, syphilis progresses to the latent stage.
- The bacterium remains in the body, but there are no visible symptoms.
- Latent syphilis is further divided into early latent (within the first year of infection) and late latent (after one year).
- Tertiary Syphilis:
-
- Develops in a subset of individuals if the infection progresses beyond the latent stage.
- Tertiary syphilis can lead to severe complications, affecting the heart, brain, nerves, and other organs.

Syphilis is diagnosed through blood tests, such as the Rapid Plasma Reagin (RPR) and Venereal Disease Research Laboratory (VDRL) tests, which detect antibodies produced in response to the infection. It is treatable with antibiotics, usually penicillin. Early detection and treatment are crucial to prevent disease progression and potential complications. Safe sexual practices, including condom use, can reduce the risk of syphilis transmission.
Treatment of Syphilis
The primary treatment for syphilis involves the use of antibiotics, with penicillin being the preferred and most effective choice. The specific antibiotic and duration of treatment depend on the stage of syphilis:
- Early Syphilis (Primary and Secondary):
-
- Intramuscular injection of benzathine penicillin G is the standard treatment.
- Alternative antibiotics such as doxycycline or tetracycline may be used in individuals with penicillin allergies.
- Latent Syphilis and Tertiary Syphilis:
-
- Benzathine penicillin G is also the preferred treatment, but the duration of treatment may be extended based on the duration of infection.
- Neurosyphilis:
-
- Intravenous penicillin G is often required for cases involving the central nervous system.
- Follow-Up and Monitoring:
-
- Individuals treated for syphilis should undergo regular follow-ups to ensure the effectiveness of the treatment.
- Testing for cure involves monitoring serological markers, such as the Venereal Disease Research Laboratory (VDRL) or Rapid Plasma Reagin (RPR) tests.
It’s crucial for individuals diagnosed with syphilis to complete the full course of prescribed antibiotics as directed by healthcare professionals. Additionally, partners of individuals with syphilis should be tested and treated if necessary to prevent further transmission. Regular follow-up and testing are essential to monitor for potential reinfection and ensure successful treatment.
What is HIV?
HIV, or Human Immunodeficiency Virus, is a retrovirus that attacks the immune system, specifically the CD4 cells (T cells), which play a crucial role in the body’s defense against infections and diseases. HIV can lead to the disease AIDS (Acquired Immunodeficiency Syndrome) if not properly treated.
Key points about HIV:
- Transmission:
-
- HIV is primarily transmitted through unprotected sexual intercourse (vaginal, anal, or oral) with an infected person.
- It can also be transmitted through contact with infected blood, sharing needles or syringes, and from mother to child during childbirth or breastfeeding.
- Clinical Stages:
-
- Acute HIV Infection: The initial stage, often accompanied by flu-like symptoms, occurs shortly after infection.
- Clinical Latency: Asymptomatic stage where the virus replicates at low levels.
- AIDS (Acquired Immunodeficiency Syndrome): The final stage, characterized by severe immune system damage and the onset of opportunistic infections or cancers.
- Symptoms:
-
- Early infection may present flu-like symptoms such as fever, fatigue, and sore throat.
- As the disease progresses, symptoms may include weight loss, recurrent infections, night sweats, and swollen lymph nodes.
- Diagnosis:
-
- HIV is diagnosed through blood tests that detect the presence of antibodies or viral genetic material (RNA).
- Common tests include ELISA (enzyme-linked immunosorbent assay) and Western blot for antibody detection, as well as PCR (polymerase chain reaction) for viral RNA.

Early detection, access to medical care, and adherence to treatment regimens are crucial for managing HIV and preventing the progression of AIDS. Regular testing, safer sex practices, and community support play key roles in HIV prevention and control.
Prevention of HIV
- Safe Sex Practices:
-
- Consistent and correct use of condoms during sexual intercourse reduces the risk of HIV transmission.
- Pre-Exposure Prophylaxis (PrEP):
-
- PrEP involves taking daily medication (usually a combination of tenofovir and emtricitabine) to reduce the risk of HIV infection, especially for individuals at higher risk.
- Needle Exchange Programs:
-
- Providing clean needles and syringes to individuals who use injectable drugs helps prevent the spread of HIV through shared needles.
- Education and Awareness:
-
- Public education campaigns to increase awareness about HIV transmission, prevention methods, and the importance of testing.
- Testing and Counseling:
-
- Regular testing for HIV and early detection allows for timely medical intervention and prevention of further transmission.
- Counseling services to promote safer sex practices and address psychosocial aspects of HIV.
- Treatment of Sexually Transmitted Infections (STIs):
-
- Treating other STIs promptly can reduce the risk of HIV transmission, as some STIs increase susceptibility.
- Medical Male Circumcision:
-
- Studies have shown that male circumcision can reduce the risk of HIV transmission from females to males.
Treatment of HIV
- Antiretroviral Therapy (ART):
-
- ART is the primary treatment for HIV.
- Combination drug regimens suppress the replication of the virus, allowing the immune system to recover and reducing the risk of transmission.
- Early initiation of ART is crucial for better outcomes.
- Adherence to Medication:
-
- Strict adherence to the prescribed medication schedule is essential for the effectiveness of ART.
- Skipping doses or inconsistent use can lead to drug resistance.
- Monitoring and Follow-Up:
-
- Regular monitoring of viral load and CD4 cell count to assess the effectiveness of treatment.
- Ongoing medical follow-up to manage side effects and adjust treatment if necessary.
- Preventing Opportunistic Infections:
-
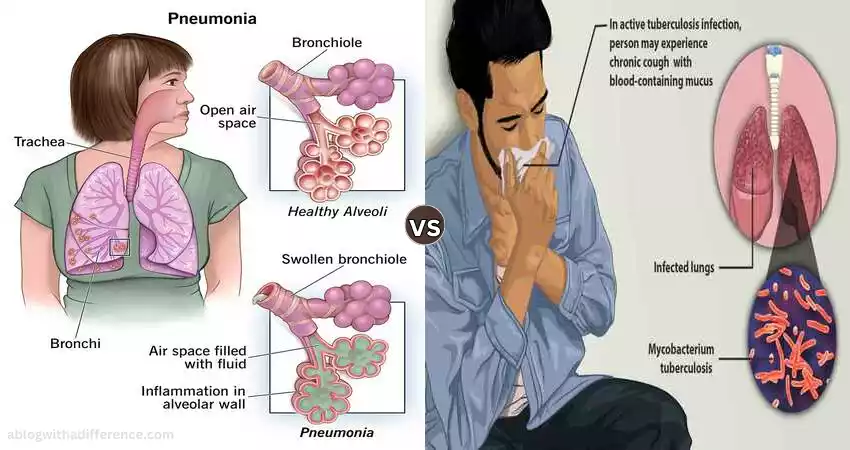
- Prophylactic treatment to prevent opportunistic infections, such as Pneumocystis pneumonia or Mycobacterium avium complex.
- Supportive Care:
-
- Nutritional support, mental health services, and other supportive care measures to enhance overall well-being.
- Preventing Mother-to-Child Transmission:
-
- Administering antiretroviral drugs to pregnant women with HIV and providing appropriate interventions during childbirth and breastfeeding to prevent transmission to the child.
- Vaccinations:
-
- Ensuring that individuals with HIV receive recommended vaccinations to prevent additional infections.
- Treatment as Prevention (TasP):
-
- Effective treatment not only improves the health of individuals with HIV but also reduces the likelihood of transmitting the virus to others.
A comprehensive approach to HIV involves a combination of prevention strategies, early detection, and access to appropriate medical care. Education, community support, and the reduction of stigma around HIV contribute to successful prevention and treatment efforts.
Syphilis and HIV in the comparison chart
| Aspect | Syphilis | HIV (Human Immunodeficiency Virus) |
|---|---|---|
| Causative Agent | Bacterium – Treponema pallidum | Retrovirus – HIV-1 and HIV-2 |
| Transmission | Sexual contact, vertical transmission (mother to child), rare cases through non-sexual contact | Sexual contact, parenteral transmission (sharing needles), vertical transmission (mother to child) |
| Clinical Stages | Primary, secondary, latent, tertiary | Acute infection, clinical latency, AIDS |
| Symptoms | Primary: painless sores; Secondary: rash, mucous membrane lesions; Latent: asymptomatic; Tertiary: severe organ damage | Initial: flu-like symptoms; Later: opportunistic infections, weight loss, night sweats |
| Diagnostic Methods | Serologic tests (RPR, VDRL), microscopic examination of lesions | Antibody tests (ELISA, Western blot), nucleic acid tests (PCR) |
| Treatment | Antibiotics (usually penicillin) | Antiretroviral therapy (ART) |
| Prevention | Safe sexual practices, condom use, partner notification and treatment | Safe sexual practices, condom use, PrEP (pre-exposure prophylaxis), needle exchange programs |
| Stigma and Perception | The stigma associated with historical misconceptions; perception influenced by awareness campaigns | Stigma is historically associated with certain groups; awareness campaigns aim to reduce stigma |
| Prevalence | Global prevalence with regional variations | Global epidemic affecting millions worldwide |
| Vaccine | No vaccine available | No cure or vaccine; PrEP for prevention |
| Public Health Impact | This can lead to outbreaks, economic burden, and severe complications if untreated | Global impact on morbidity, mortality, economic and social aspects; requires extensive public health resources |
| Community Support | Support groups and education campaigns aimed at reducing stigma and promoting testing | Extensive network of support groups, advocacy, and awareness organizations |
This comparison chart provides a brief overview of key aspects related to syphilis and HIV, highlighting differences in causative agents, transmission, clinical stages, diagnostic methods, treatment, prevention, public health impact, and community support. It is important to note that each infection presents unique challenges, and individual experiences may vary.
Impact on Public Health
The impact of syphilis and HIV on public health includes:
Syphilis:
- Transmission and Spread:
-
- Uncontrolled transmission can lead to outbreaks and increased prevalence within communities.
- Congenital Syphilis:
-
- Maternal transmission can result in serious health issues for infants, including stillbirth or severe complications.
- Economic Burden:
-
- Treatment costs and the management of complications contribute to the economic burden on healthcare systems.
- Public Awareness:
-
- Lack of awareness may lead to delayed diagnosis and treatment, exacerbating the impact on individuals and public health.
HIV:
- Epidemic Scale:
-
- HIV has been a global epidemic, affecting millions of people worldwide and posing significant challenges for public health systems.
- Morbidity and Mortality:
-
- AIDS-related illnesses can lead to increased morbidity and mortality rates, affecting overall population health.
- Stigma and Discrimination:
-
- The stigma associated with HIV can hinder prevention efforts, discourage testing, and contribute to discrimination against affected individuals.
- Social and Economic Consequences:
-
- HIV affects workforce productivity and family structures, contributing to social and economic challenges within communities.
- Healthcare Resource Allocation:
-
- Managing HIV requires substantial healthcare resources, diverting attention and resources from other health priorities.
- Prevention Challenges:
-
- Ongoing prevention efforts face challenges related to risk behavior, awareness, and access to preventive measures.
Common Challenges:
- Co-Infection Risk:
-
- Individuals with syphilis or other STIs may be at a higher risk of contracting or transmitting HIV, highlighting the interconnectedness of these public health challenges.
- Health Inequalities:
-
- Both syphilis and HIV disproportionately affect marginalized and vulnerable populations, exacerbating existing health inequalities.
Addressing syphilis and HIV requires comprehensive public health strategies, including awareness campaigns, prevention education, widespread testing, early diagnosis, and accessible treatment. Efforts to reduce stigma, promote safe practices, and ensure equitable access to healthcare resources are crucial for mitigating the impact of these infections on public health.
Misconceptions and Myths
Misconceptions and Myths about Syphilis:
- Myth: Syphilis only affects certain demographics.
- Fact: Syphilis can affect anyone, regardless of age, gender, or socioeconomic status.
- Myth: Syphilis can only be transmitted through sexual intercourse.
- Fact: While sexual contact is a common mode of transmission, syphilis can also be transmitted from mother to child during childbirth and through direct contact with syphilis sores.
- Myth: Syphilis always presents with noticeable symptoms.
- Fact: Syphilis can be asymptomatic in its early stages, making regular testing crucial for detection.
- Myth: Syphilis is not a serious or life-threatening infection.
- Fact: Untreated syphilis can progress to severe stages, affecting various organs and causing significant health complications.
Misconceptions and Myths about HIV:
- Myth: HIV can be cured by alternative therapies or natural remedies.
- Fact: There is no cure for HIV, and antiretroviral therapy is the standard treatment to manage the infection.
- Myth: You can contract HIV from sharing utensils or toilet seats.
- Fact: HIV is not transmitted through sharing everyday items like utensils or toilet seats.
- Myth: HIV only affects specific populations, such as men who have sex with men.
- Fact: HIV can affect anyone, regardless of sexual orientation, gender, or demographic factors.
Common Misconceptions:
- Misconception: Syphilis and HIV are the same.
- Fact: Syphilis and HIV are distinct infections caused by different pathogens, transmitted differently, and with different clinical courses.
- Misconception: You can’t get syphilis or HIV if you’re in a monogamous relationship.
- Fact: Monogamous individuals can still contract these infections if their partner is infected or if preventive measures are not taken.
- Misconception: Syphilis and HIV are only concerns for certain “high-risk” groups.
- Fact: Everyone is at risk, and awareness and prevention are important for everyone, regardless of perceived risk.
Addressing these misconceptions is crucial for fostering accurate understanding, promoting preventive measures, and reducing the stigma associated with syphilis and HIV. Education campaigns and open communication can play a significant role in dispelling myths and promoting factual information.
Risk Factors
Risk Factors for Syphilis
- Unprotected Sexual Activity:
-
- Engaging in sexual intercourse without using condoms increases the risk of syphilis transmission.
- Multiple Sexual Partners:
-
- Having multiple sexual partners, especially without consistent condom use, elevates the risk of exposure to syphilis and other sexually transmitted infections.
- Men who have sex with men (MSM):
-
- MSM are at an increased risk of syphilis transmission due to higher rates of certain sexual practices.
- Illicit Drug Use:
-
- Sharing needles or drug paraphernalia increases the risk of syphilis transmission.
- HIV Infection:
-
- Individuals with HIV are at an increased risk of syphilis and may experience more severe manifestations of the infection.
- Age:
-
- Young adults and individuals in their reproductive years have a higher risk of syphilis.
- Geographical Location:
-
- Syphilis prevalence can vary by region, and areas with higher rates of infection pose an increased risk.
Risk Factors for HIV
- Unprotected Sexual Activity:
-
- Engaging in sexual intercourse without using condoms, particularly with multiple partners or individuals with unknown HIV status.
- Sharing Needles:
-
- Intravenous drug users who share needles or syringes are at a higher risk of HIV transmission.
- Vertical Transmission:
-
- Pregnant women with HIV can transmit the virus to their infants during childbirth or breastfeeding.
- Sexually Transmitted Infections (STIs):
-
- Having other STIs, especially those that cause genital sores or inflammation, increases susceptibility to HIV.
- HIV-Positive Partners:
-
- Engaging in sexual activity with a partner who is HIV-positive without using preventive measures.
- Men who Have Sex with Men (MSM):
-
- MSM have a higher risk of HIV transmission due to the higher prevalence of the virus in this population.
- Geographical Location:
-
- HIV prevalence varies by region, and areas with higher rates pose an increased risk.
- Age:
-
- Young adults and individuals in their reproductive years are at a higher risk of HIV.
Common Risk Factors
- Lack of Awareness:
-
- Individuals who are not informed about the risks of syphilis and HIV may engage in behaviors that increase their likelihood of infection.
- Stigma and Discrimination:
-
- The stigma surrounding syphilis and HIV may discourage individuals from seeking testing, treatment, or preventive measures.
- Limited Access to Healthcare:
-
- Lack of access to healthcare services, including testing and treatment, can contribute to the spread of syphilis and HIV.
- Economic Disparities:
-
- Individuals facing economic challenges may have limited access to preventive measures and healthcare resources.
- Substance Abuse:
-
- Substance abuse, including alcohol and drug use, can contribute to risky behaviors that increase the risk of syphilis and HIV.
Understanding these risk factors is crucial for developing targeted prevention strategies, public health campaigns, and educational initiatives to reduce the incidence of syphilis and HIV. Encouraging regular testing, promoting safe sex practices, and addressing social determinants of health contribute to effective risk reduction.
The Importance of Regular Testing
Importance of Regular Testing for Syphilis:
- Early Detection and Treatment:
-
- Regular testing allows for the early detection of syphilis, enabling prompt treatment and reducing the risk of complications.
- Preventing Transmission:
-
- Individuals who know their syphilis status can take preventive measures to avoid transmitting the infection to their sexual partners.
- Identifying Asymptomatic Cases:
-
- Syphilis can be asymptomatic, meaning individuals may not exhibit noticeable symptoms. Regular testing helps identify cases with no apparent signs.
- Preventing Congenital Syphilis:
-
- Testing and treating pregnant women for syphilis prevent the transmission of the infection to their infants, reducing the risk of congenital syphilis.
- Partner Notification and Treatment:
-
- Individuals who test positive can inform their sexual partners, encouraging them to seek testing and treatment, thus preventing further transmission.
Importance of Regular Testing for HIV:
- Early Diagnosis and Treatment:
-
- Early detection of HIV through regular testing allows for timely initiation of antiretroviral therapy (ART), improving health outcomes.
- Preventing Disease Progression:
-
- Early treatment helps prevent the progression of HIV to AIDS and reduces the risk of opportunistic infections and complications.
- Protecting Sexual Partners:
-
- Individuals aware of their HIV status can take steps to prevent transmission to their sexual partners, such as using condoms and practicing safer sex.
- Preventing Mother-to-Child Transmission:
-
- Regular testing and treatment during pregnancy prevent the transmission of HIV from mother to child.
- Behavioral Changes:
-
- Knowing one’s HIV status may lead to behavioral changes that reduce the risk of engaging in high-risk activities.
- Improving Overall Health:
-
- Regular monitoring of HIV allows healthcare providers to manage associated health issues and promote overall well-being.
Regular testing for syphilis and HIV is a fundamental aspect of individual and public health. It empowers individuals to make informed decisions about their sexual health, facilitates early intervention, and plays a crucial role in preventing the spread of these infections within communities.
Living with Syphilis or HIV
Living with syphilis or HIV involves comprehensive medical care, emotional support, and lifestyle adjustments. Here are key aspects of living with each condition:
Living with Syphilis:
- Medical Management:
-
- Syphilis is treatable with antibiotics, usually penicillin. Following the prescribed treatment plan is essential.
- Regular follow-up appointments and testing are crucial to monitor treatment effectiveness and prevent complications.
- Partner Communication:
-
- Informing sexual partners about the infection is important for their health and to prevent further transmission.
- Partners should be encouraged to seek testing and treatment as well.
- Preventing Reinfection:
-
- Individuals treated for syphilis should take precautions to avoid reinfection, such as practicing safe sex and addressing lifestyle factors that may contribute to recurrence.
- Psychosocial Support:
-
- Coping with a syphilis diagnosis may involve emotional challenges. Seeking support from friends, family, or mental health professionals can be beneficial.
- Preventing Congenital Syphilis:
-
- For pregnant individuals, seeking early prenatal care and testing is crucial to prevent transmission to the unborn child.
Living with HIV:
- Antiretroviral Therapy (ART):
-
- Individuals with HIV are typically prescribed ART to manage the virus and maintain a healthy immune system.
- Adhering to the medication regimen is essential for treatment success.
- Regular Medical Monitoring:
-
- Regular check-ups and monitoring of viral load and CD4 cell count are essential components of HIV management.
- Preventing Opportunistic Infections:
-
- Following healthcare provider recommendations for vaccinations and prophylactic medications helps prevent opportunistic infections.
- Lifestyle Adaptations:
-
- Adopting a healthy lifestyle, including a balanced diet, regular exercise, and adequate sleep, can support overall well-being.
- Emotional Support:
-
- Living with HIV can be emotionally challenging. Seeking support from friends, family, support groups, or mental health professionals can be beneficial.
- Preventing Transmission:
-
- Taking precautions to prevent the transmission of HIV to sexual partners, such as practicing safe sex and disclosing one’s status, is crucial.
- Community Engagement:
-
- Involvement in supportive communities and advocacy groups can provide a sense of belonging and empowerment.
Living with syphilis or HIV is manageable with proper medical care, support, and a proactive approach to health. Regular communication with healthcare providers, adherence to treatment plans, and a holistic approach to well-being contribute to a fulfilling and healthy life despite these diagnoses.
Conclusion
In conclusion, living with syphilis or HIV requires a multifaceted approach that includes medical management, emotional support, and lifestyle adjustments. Early detection, adherence to treatment, and regular monitoring are crucial for managing these conditions effectively.
Additionally, open communication with healthcare providers, partners, and support networks, along with efforts to reduce stigma and increase awareness, play pivotal roles in fostering a healthy and fulfilling life for individuals with syphilis or HIV. Regular testing, safe sex practices, and community engagement contribute to overall well-being and prevention efforts.
FAQs
Q1: Can syphilis or HIV be cured?
A: Syphilis is curable with antibiotics, especially in its early stages. HIV is not curable, but antiretroviral therapy (ART) can effectively manage the virus, allowing individuals to lead healthy lives.
Q2: How often should I get tested for syphilis and HIV?
A: The frequency of testing depends on individual risk factors. Sexually active individuals, those with multiple partners, or individuals engaging in high-risk behaviors should consider regular testing, ideally at least annually.
Q3: Can I live a normal life with HIV or syphilis?
A: Yes, with proper medical care and adherence to treatment plans, individuals with HIV or syphilis can lead normal and fulfilling lives. Regular monitoring, lifestyle adjustments, and emotional support are essential components of managing these conditions.
Q4: How is syphilis transmitted?
A: Syphilis is primarily transmitted through sexual contact, including vaginal, anal, or oral sex. It can also be transmitted from mother to child during childbirth or pregnancy.
Q5: Is it possible to prevent syphilis or HIV?
A: Yes, both infections can be prevented. Safe sex practices, consistent condom use, regular testing, and, in the case of HIV, pre-exposure prophylaxis (PrEP) can significantly reduce the risk of transmission.
Q6: Are there support groups for people with syphilis or HIV?
A: Yes, various support groups, community organizations, and online platforms provide support for individuals living with syphilis or HIV. These groups offer emotional support, information, and a sense of community.
Q7: Can I have a healthy relationship if I have syphilis or HIV?
A: Yes, individuals with syphilis or HIV can have healthy relationships. Open communication, safe sex practices, and partner education are essential for maintaining healthy relationships while managing these conditions.
Q8: Is there a vaccine for syphilis or HIV?
A: There is no vaccine for syphilis. While there is no vaccine for HIV, pre-exposure prophylaxis (PrEP) can be taken by individuals at high risk to reduce the likelihood of HIV transmission.
These FAQs provide brief answers, but individuals are encouraged to consult healthcare professionals for personalized information and guidance based on their specific circumstances.