Difference Between Ganglion Cyst and RA Nodule
Overview of Ganglion Cyst and RA Nodule
Ganglion Cyst and RA Nodule are lumps or swellings that can develop near joints. Ganglion cysts are noncancerous fluid-filled lumps that usually appear near joints or tendons most frequently in the wrist or hand and usually remain painless.
Though pressing on nearby structures could potentially cause discomfort and limit joint movement. They’re considered non-inflammatory in nature and are likely due to accumulations of synovial fluid lubricating joints often called synovial fluid.
An RA nodule is a firm, round lump that appears in individuals suffering from rheumatoid arthritis (RA), an autoimmune condition characterized by chronic joint inflammation. Composed of immune cells, these nodules usually form under or near joints affected by RA; unlike ganglion cysts, they are usually painful and indicative of underlying autoimmunity processes in this disease.
Explanation of Ganglion Cyst
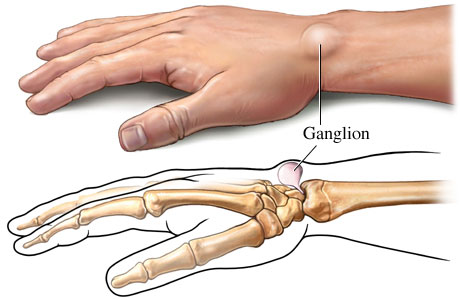
Ganglion cysts are noncancerous lumps that often arise near joints or tendons, most often in the wrist or hand but sometimes ankle or foot. Ganglion cysts can appear anywhere along these areas and typically display round or oval shapes filled with a jelly-like fluid.
Although their exact cause remains elusive, many researchers suspect they form due to leakage of synovial fluid, the lubricating fluid found within joints that accumulates and accumulates into cystic structures over time. While usually painless, ganglion cysts may press on nearby nerves or hinder joint movement causing discomfort or even pain.
One notable feature of ganglion cysts is their variable size over time. If a joint experiences increased activity or rest, it may swell larger. Otherwise, it may shrink with rest. Some individuals choose to leave these cysts untreated if they do not cause significant pain or functional impairment. Otherwise, treatments include aspiration (using a needle to drain fluid away) and surgical removal if the cyst recurs or persists.
Ganglion cysts are generally harmless. To ensure accurate diagnosis and evaluation by healthcare professionals and determine an effective plan of management. Accurate diagnosis may help rule out more serious conditions or determine the appropriate action to take for managing this cyst.
Signs and symptoms
- Visible Lump: Ganglion cysts usually manifest themselves as visible lumps or bumps on the skin’s surface near joints or tendons, typically round or oval in shape.
- Painless Swelling: Ganglion cysts tend to be painless; however, they may occasionally cause mild discomfort or ache if they press against nearby nerves or tissues.
- Size Variability: Over time, the cyst may experience fluctuation. With increased joint activity or trauma it may become larger while when rest is given it can diminish in size.
- Translucency: Ganglion cysts often have an opaque or semi-translucent appearance that allows you to see through to their inner fluid or gel-like material, giving a glimpse into their interior structure.
- Restricting Joint Movement: If a cyst is pressing against adjacent structures or impinging upon a joint, its range of motion may become limited.
- Tenderness Around Ganglion Cyst: When inflammation or irritation are present, the area surrounding a ganglion cyst may become tender to touch.
- Possible Changes in Skin Color: The skin surrounding a cyst may remain normal or develop slight discolorations or reddening in some instances.
Causes of ganglion cysts
- Ganglion Cysts Caused by Joint or Tendon Irritation: Ganglion cysts may develop due to joint irritation or minor trauma. Repetitive microtrauma or mechanical stress to a joint or tendon can trigger their development into cysts.
- Synovial Fluid Accumulation: Ganglion cyst formation can be explained by leakage of synovial fluid from its home in the joint into surrounding tissues and its accumulation into cystic structures.
- Idiopathic: Sometimes the source of ganglion cysts remains unclear; when this is the case, they are known as “idiopathic”, meaning they form without apparent cause.
Explanation of RA Nodule

An Rheumatoid Arthritis nodule, also known as an RA nodule, is an iconic feature of Rheumatoid Arthritis (RA), an autoimmune condition primarily affecting joints. Nodules often appear under skin layers near joints or organs – typically painlessly but may occasionally become tender and inflamed.
Nodules in RA are composed of immune cells and fibrous tissue and result from chronic inflammation associated with this condition. They typically appear on areas exposed to repeated mechanical stress such as the elbows, fingers, or heels but may appear elsewhere too. Nodules can range in size from small pea-sized bumps to larger, more noticeable lumps.
Nodules in RA are not directly responsible for joint damage, they are an important symptom and often indicate more severe forms. Their presence can reduce joint function and cosmetic issues, with treatment typically consisting of using disease-modifying antirheumatic drugs (DMARDs) to manage inflammation and joint damage.
In certain instances, surgical removal may be considered in cases of nodules that become symptomatic; regardless, managing RA overall is key in order to address both its nodule manifestations as well as any wider impacts it might have on joint health and overall well-being.
Signs and symptoms
- Firm Lumps: Nodules caused by RA often appear as firm, raised lumps beneath the skin near joints or areas subjected to repeated mechanical stress.
- Tenderness: Nodules can become sensitive or painful when they press on nearby nerves and tissues, especially when pressing against nerve endings or tissues.
- Joint Symptoms: Nodules associated with RA are often seen alongside other signs and symptoms of joint disease, including pain, swelling, stiffness and stiffness in joints. Furthermore, nodules can appear concurrently with joint inflammation.
- Size Variability: Nodules caused by RA can range in size, from small pea-sized nodules to larger lumps that become noticeable over time.
- Redness in Skin Overlying Nodules: Inflamed or irritated nodules may cause their surrounding skin to turn red or discolor, creating reddened patches overlying them that could eventually turn purple in appearance.
- Mobility Limits: Nodules can cause mobility restrictions that interfere with daily activities and could limit joint movement, impacting day-to-day living and activities.
- Chronic Course: Nodules associated with RA are typically characteristic of more aggressive disease conditions and should serve as an early warning signal of disease progression.
Causes of RA Nodules
- Causes of RA Nodules: Rheumatoid Arthritis (RA): Nodules associated with Rheumatoid Arthritis, an autoimmune disease, are due to its associated dysfunction of the immune system and result from this state.
- Autoimmune Reaction: With RA, the immune system mistakenly attacks healthy joint tissues resulting in chronic inflammation that over time may lead to nodule formation.
- Severity of Rheumatoid Arthritis: Rheumatoid nodules are more often observed in individuals who have severe or longstanding Rheumatoid Arthritis, suggesting a relationship between the disease’s progression and these nodules’ appearance.
key differences between Ganglion cysts and RA nodules
Here’s a comparison chart summarizing the key differences between ganglion cysts and RA nodules:
| Characteristic | Ganglion Cyst | RA Nodule |
|---|---|---|
| Etiology | Accumulation of synovial fluid | Result of chronic inflammation in Rheumatoid Arthritis |
| Pain and Inflammation | Typically painless, non-inflammatory | Can be painful and associated with RA-related inflammation |
| Location | Commonly near joints, often in the wrist or hand | Typically near joints but also found under the skin or near affected joints in Rheumatoid Arthritis |
| Appearance | Round or oval-shaped lump filled with jelly-like fluid | Firm, round or oval-shaped lump composed of immune cells and fibrous tissue |
| Underlying Condition | Not associated with any specific underlying disease | Specific to Rheumatoid Arthritis as a manifestation of the autoimmune process |
| Prognosis | Favorable, typically benign | Indicates more severe forms of Rheumatoid Arthritis; management is crucial for RA control |
| Treatment | Aspiration (draining the fluid) or surgical removal if symptomatic | Focuses on controlling underlying Rheumatoid Arthritis with medications; surgical removal for symptomatic nodules is an option |
| Recurrence | Can recur after treatment or surgical removal | May persist or recur if RA is not effectively managed |
| Functional Impact | Rarely affects joint function | Can sometimes impact joint function, especially if located near joints |
| Cosmetic Concerns | May or may not be cosmetically bothersome | Can be a cosmetic concern due to their visibility |
| Diagnostic Methods | Physical examination, imaging studies (e.g., ultrasound, MRI) | Clinical evaluation within the context of Rheumatoid Arthritis diagnosis |
| Association with Other Conditions | Generally not associated with other medical conditions | Occurs as part of the RA disease process and is specific to RA |
Diagnosis Method
How to diagnose ganglion cysts
Medical History and Physical Examination:
- Your healthcare provider will begin by gathering an extensive medical history. They may ask about symptoms, when and how you first noticed the lump, as well as any associated pain or discomfort.
- An extensive physical exam will be performed during which the healthcare provider will assess the size, location and characteristics of any lumps present, as well as any signs of tenderness or joint limitations.
Imaging Studies:
- Diagnostic imaging such as ultrasound or magnetic resonance imaging (MRI) may be ordered to detect and visualize ganglion cysts, their size, location and relationship to nearby structures. Ultrasound may be best as it allows clinicians to distinguish ganglion cysts from other lumps or masses more readily.
Aspiration (optional):
- Your healthcare provider may recommend aspirating the ganglion cyst to remove excess fluid. A fine needle will then be used to withdraw this liquid. Aspiration serves both diagnostic and therapeutic functions. It helps confirm diagnosis while also offering temporary relief from symptoms if your cyst is painful. As well, aspiration provides confirmation of diagnosis while simultaneously alleviating painful symptoms associated with the ganglion cyst.
Differential Diagnosis:
- Healthcare providers will first rule out other conditions that might resemble ganglion cysts, such as lipomas, hernias or other cysts or tumors. Consultation with a Specialist
(Optional):
- Based on the complexity or location of your cyst, depending on
- its complexity or location you may be referred to a specialist like an orthopedic surgeon or hand surgeon for further evaluation and treatment planning.
How to diagnose RA nodules
Medical History and Physical Examination:
- Your healthcare provider will begin by reviewing a thorough medical history, taking note of symptoms you are currently experiencing as well as the duration and onset. He or she may also inquire into any family histories for autoimmune disease that exist in either you or the immediate family.
- A physical examination should include an assessment of joint involvement, tender or swollen joints and skin nodule detection. Laboratory Tests: Blood tests are an integral component of diagnosing RA and its nodules.
Laboratory Tests:
- Rheumatoid Factor (RF) and Anti-CCP Antibodies: Elevated levels of these autoantibodies are common among those suffering from RA, providing evidence to support a diagnosis.
- C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR): Elevated levels of these markers indicate inflammation associated with RA.
- Complete Blood Count (CBC): Anemia has also been associated with this disorder.
Imaging Studies:
- X-rays, ultrasound, or magnetic resonance imaging (MRI) studies may be utilized to assess joint damage and inflammation as well as visualize any nodules located near the joints.
Clinical Criteria:
- Diagnosing arthritis typically relies on established clinical criteria, such as those found in the 2010 American College of Rheumatology/European League Against Rheumatism classification criteria for RA. These include joint involvement, blood test results, and duration of symptoms as some key points.
Biopsy (Optional):
- To ensure accurate diagnosis of an RA nodule, in some instances, a biopsy may be conducted to obtain tissue samples for examination under a microscope to assess their unique features.
Consultation with a Rheumatologist:
- Rheumatologists specialize in treating autoimmune and inflammatory conditions, such as arthritis (RA). If your healthcare provider suspects RA or nodules on you, they may refer you to a rheumatologist for further evaluation and management.
Treatment Options
Treatment of Ganglion Cysts
- Observation: Ganglion cysts that don’t cause discomfort or functional limitations should likely go untreated, with periodic monitoring by healthcare providers to check for changes in size or symptoms.
- Aspiration: If the cyst is painful or causing discomfort, aspiration may provide temporary relief; during this procedure a fine needle is used to drain away fluid from it using aspiration. Aspiration can provide short-term relief; however, cysts may recur.
- Corticosteroid Injection (Optional): For some cysts, an additional corticosteroid injection may be prescribed to reduce inflammation and help avoid future cyst recurrence.
- Splinting or Bracing: Wearing a splint or brace may be recommended in certain instances to temporarily immobilize the affected joint and minimize irritation to its cyst.
- Surgery: When large cysts become painful or significantly reduce functionality, surgery to remove them may be an option. This procedure typically requires orthopedic or hand surgeons and includes excising not only the cyst itself but also a portion of the joint capsule or tendon sheath as a precautionary measure against future recurrences.
Treatment of RA Nodules
- Disease-Modifying Antirheumatic Drugs (DMARDs): The key component of treating RA nodules lies in controlling inflammation and joint damage associated with Rheumatoid Arthritis; therefore DMARDs like methotrexate, sulfasalazine, and biologic agents like TNF inhibitors may be prescribed to reduce inflammation and joint destruction and indirectly help decrease size or formation of nodules.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Nonsteroidal anti-inflammatory drugs may help alleviate pain and inflammation associated with RA nodules.
- Corticosteroids: Intralesional corticosteroid injections may be administered directly into nodules to reduce their size and alleviate discomfort, while systemic corticosteroids may also be prescribed in cases of acute flare-ups.
- Surgery (Rarely): Surgery may be used to address nodules that cause severe discomfort, ulceration or functional impairment and have not responded well to other treatments.
- Biologic Agents: When treating nodules that refract, biologic medications like Rituximab or Abatacept may be considered as possible solutions.
- Consultation With a Rheumatologist: Individuals diagnosed with nodules of RA should seek the care of a rheumatologist in order to develop customized plans to treat both their nodules and underlying RA effectively.
Ending
Ganglion cysts are non-inflammatory, fluid-filled lumps commonly seen near joints in the wrist or hand. Rheumatoid Arthritis nodules are firm, inflammatory lumps associated with Rheumatoid Arthritis (RA). Ganglion cysts tend to be painless.
RA nodules may be painful and indicate more severe forms of the disease; for these reasons, aspiration or surgery may be required in cases where symptoms arise while management for nodules involves treating their source RA nodules.