6 Best Difference Between Catecholamines and Acetylcholine
Catecholamines and Acetylcholine play essential roles in the human body, serving as neurotransmitters that facilitate communication between nerve cells. They have different chemical structures, are synthesized and metabolized differently, and have distinct roles in various physiological processes.
Definition of Catecholamines
Catecholamines are a class of organic compounds primarily acting as neurotransmitters in the central and peripheral nervous system. These molecules play crucial roles in the body’s physiological response to stress, often referred to as the “fight or flight” response.
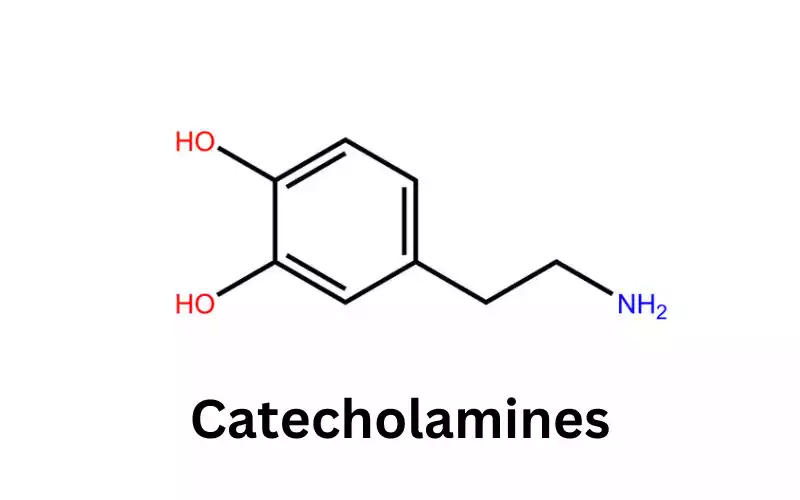
They originate from the amino acid tyrosine and include dopamine, norepinephrine (also known as noradrenaline), and epinephrine (adrenaline). Notably, catecholamines influence various bodily functions such as heart rate, blood pressure, glucose metabolism, and mood regulation.
Their release typically results from situations that induce physical or emotional stress. Dysregulation in catecholamine levels or their receptors is associated with several disorders, including Parkinson’s disease, depression, and certain types of tumors, like pheochromocytoma.
Definition of Acetylcholine
Acetylcholine (ACh) is a vital neurotransmitter in both the central and peripheral nervous systems, playing pivotal roles in muscle contraction, heart rate regulation, memory, and numerous other physiological processes.
Discovered in the early 20th century, ACh became the first neurotransmitter to be identified. It operates at the neuromuscular junction, facilitating communication between nerve cells and muscle cells. The central nervous system is involved in arousal, attention, motivation, and other cognitive functions.
In the peripheral nervous system, ACh serves as the principal neurotransmitter in the parasympathetic division, promoting “rest and digest” bodily responses. Disturbances in ACh-related systems are implicated in various conditions, including Alzheimer’s disease and myasthenia gravis.
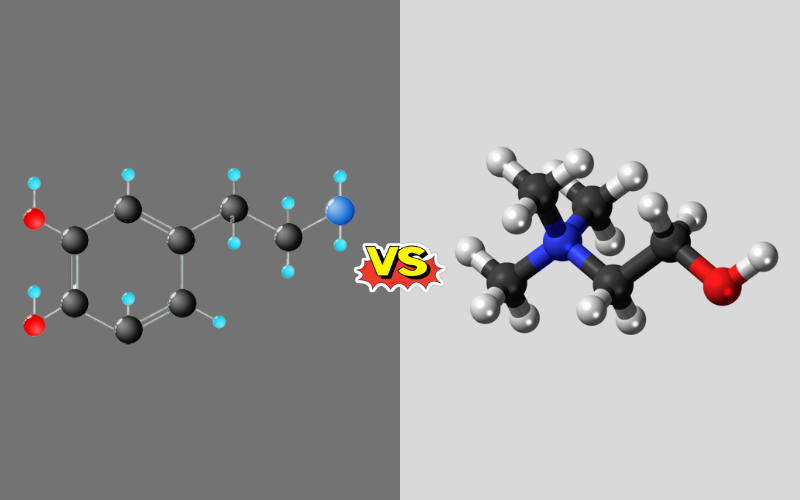
Chemical Structure of Catecholamines and Acetylcholine
Catecholamines: The term “catecholamine” is derived from the core structure known as “catechol”. Catecholamines have a common structural backbone composed of a catechol nucleus, which is a benzene ring with two adjacent hydroxyl groups, and an amine side chain.
- Dopamine: It is the simplest catecholamine, having a two-carbon side chain attached to the nitrogen of the amino group.
- Norepinephrine (Noradrenaline): It is formed by adding a hydroxyl group to the beta-carbon of dopamine’s side chain.
- Epinephrine (Adrenaline): Further modification of norepinephrine by adding a methyl group to the nitrogen atom results in epinephrine.
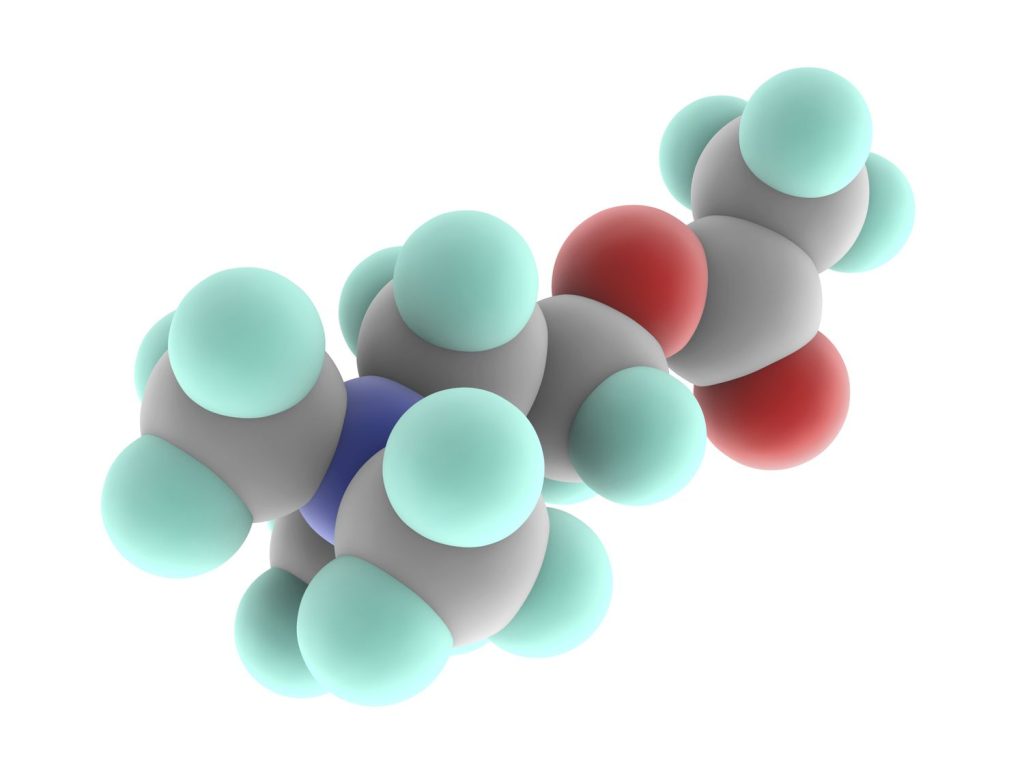
Acetylcholine: Acetylcholine is structurally distinct from catecholamines. It is composed of an ester linkage between choline and acetic acid. The molecule contains a choline portion,.
Which is a quaternary ammonium cation (having four substituents attached to the nitrogen, making it positively charged), and is attached to an acetate group. This structure is particularly suited for its function, allowing it to bind with specificity to both its nicotinic and muscarinic receptors in various parts of the body.
Physiological Roles
Catecholamines play pivotal roles in regulating mood, heart rate, blood pressure, and the “fight or flight” response. Dopamine is central to mood and motor control, norepinephrine affects attention and arousal, and epinephrine readies the body for rapid action during stress.
Acetylcholine is fundamental in neuromuscular signaling, ensuring muscle contraction. In the brain, it’s linked with arousal, attention, memory, and motivation. Additionally, the peripheral nervous system primarily facilitates “rest and digest” functions by acting as a key player in the parasympathetic nervous system.
Synthesis and Metabolism
Catecholamines are synthesized from the amino acid tyrosine. Initially, tyrosine undergoes hydroxylation to form dihydroxyphenylalanine (DOPA) through the enzyme tyrosine hydroxylase. DOPA is then decarboxylated to produce dopamine.
Dopamine can be further hydroxylated to norepinephrine and then methylated to form epinephrine. The enzymes involved in catecholamine breakdown are monoamine oxidase (MAO) and catechol-O-methyltransferase (COMT), transforming them into inactive metabolites excreted in the urine.
Acetylcholine is synthesized from choline and acetyl coenzyme A through the action of the enzyme choline acetyltransferase. Its degradation is swift, achieved by the enzyme acetylcholinesterase, which breaks it down into choline and acetate, ensuring rapid cessation of its action post-release.
Key Difference between Catecholamines and Acetylcholine
| Feature | Catecholamines | Acetylcholine |
|---|---|---|
| Components | Dopamine, Norepinephrine, Epinephrine | N/A |
| Origin | Derived from amino acid tyrosine | Synthesized from choline and acetyl coenzyme A |
| Major Roles | Mood regulation, stress response, cardiovascular regulation | Muscle contraction, cognitive function, parasympathetic activities |
| Primary Degradation Enzymes | MAO, COMT | Acetylcholinesterase |
| Associated Disorders | Parkinson’s, pheochromocytoma, mood disorders | Alzheimer’s, myasthenia gravis |
| Therapeutic Uses | Treats heart failure, shock, anaphylactic shock | Used indirectly via agents affecting its activity for Alzheimer’s, neuromuscular disorders |
Similarity of Catecholamines and acetylcholine
Catecholamines and acetylcholine are both neurotransmitters, fundamental chemicals that enable communication between nerve cells. They each play vital roles in maintaining the body’s homeostasis and ensuring proper function of the nervous system.
Both types of neurotransmitters are synthesized in the body from amino acids or their derivatives and are broken down by specific enzymes to halt their action and maintain neural balance.
Irregularities in the levels or function of either catecholamines or acetylcholine can lead to distinct neurological or physiological disorders, underscoring their importance.
Both have been the focus of numerous therapeutic interventions, with drugs targeting their synthesis, action, or degradation offering relief for various conditions.
Catecholamines and Acetylcholine Implications for Neurological Disorders
Catecholamines and acetylcholine are integral to neurological function, and imbalances often lead to disorders. For catecholamines, dopamine deficiency is paramount in Parkinson’s disease, where decreased dopamine in the basal ganglia causes tremors and rigidity.
High dopamine levels, on the other hand, are implicated in schizophrenia, where overactivity in certain brain pathways leads to hallucinations and delusions. Norepinephrine imbalances are associated with mood disorders, such as depression, due to their role in arousal and stress response.
Acetylcholine, central to neuromuscular signaling and cognitive function, when disturbed, manifests in various disorders. Alzheimer’s disease is a poignant example where cholinergic neuron degeneration in the brain leads to cognitive decline.
Myasthenia gravis, a neuromuscular disorder, arises from antibodies against acetylcholine receptors, leading to muscle weakness. Both catecholamines and acetylcholine dysfunction show the delicate balance required for the nervous system’s proper functioning.
Their respective roles in neurodegenerative and neuromuscular disorders emphasize the need for understanding their mechanisms for potential therapeutic interventions.
Catecholamines vs. Acetylcholine: Effects on the Body and Mind
Catecholamines and acetylcholine, as neurotransmitters, exert profound effects on both the body and mind. Catecholamines, particularly adrenaline, prime the body for “fight or flight” responses raising heart rate, increasing blood flow to muscles, and heightening alertness.
Dopamine, another catecholamine, deeply influences mood, motivation, and reward systems in the brain, while norepinephrine regulates attention and arousal.
Acetylcholine’s effects are multifaceted. In the peripheral nervous system, it’s indispensable for muscle contraction. A drop in acetylcholine at the neuromuscular junction, for instance, can lead to paralysis.
In the brain, it’s intricately linked with cognition regulating arousal, attention, and memory. It also drives the “rest and digest” responses in the parasympathetic nervous system.
Comparatively, while catecholamines largely drive responses to external stimuli and modulate mood and alertness, acetylcholine’s domain covers motor control, cognitive functions, and parasympathetic responses. Their interplay is complex; for example, during stress, catecholamines surge preparing the body to respond, to acetyl.
Clinical Significance
Dysregulation in catecholamine levels is associated with several disorders. Reduced dopamine levels are linked with Parkinson’s disease, while excessive levels relate to conditions like schizophrenia. Abnormalities in norepinephrine and epinephrine are tied to mood disorders and pheochromocytoma, respectively.
Alterations in acetylcholine function are significant in various conditions. Alzheimer’s disease showcases diminished cholinergic activity in the brain, leading to cognitive decline. Myasthenia gravis, a neuromuscular disorder, arises from antibodies against acetylcholine receptors, impairing muscle function.
Therapeutic Uses
Catecholamines are vital in medical interventions. Epinephrine is indispensable for anaphylactic shock, restoring heart rhythm during cardiac arrest, and acute asthma attacks. Dopamine, in pharmacological doses, treats certain types of heart failure or shock.
Acetylcholine’s therapeutic utility isn’t direct, but agents affecting its activity are valuable. Acetylcholinesterase inhibitors, like donepezil, are employed in Alzheimer’s disease, enhancing cholinergic function. In myasthenia gravis, drugs like neostigmine enhance acetylcholine availability, improving muscle strength.
Summary
Catecholamines, comprising dopamine, norepinephrine, and epinephrine, originate from tyrosine and play crucial roles in mood, stress response, and cardiovascular regulation.
Their synthesis progresses from tyrosine to dopamine, then to norepinephrine, and finally to epinephrine. Dysregulated levels can result in disorders like Parkinson’s and pheochromocytoma.
Acetylcholine, synthesized from choline and acetyl coenzyme A, is fundamental for muscle contraction, cognitive functions, and parasympathetic activities. Its degradation is rapid, ensuring quick signal termination.
Disturbances in acetylcholine activity are evident in Alzheimer’s and myasthenia gravis. Both catecholamines and acetylcholine offer therapeutic avenues; while epinephrine treats anaphylactic shock, drugs enhancing acetylcholine function help Alzheimer’s patients.