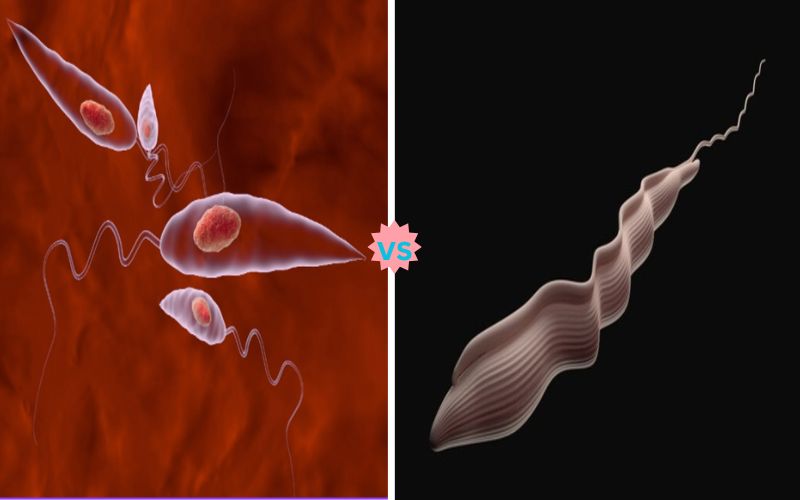
Difference Between Leishmania and Trypanosoma
Brief overview of Leishmania and Trypanosoma
Leishmania and Trypanosoma, two protozoan parasites belonging to the Kinetoplastid family of protozoa that cause significant human illnesses, are harmful protozoans known as Kinetoplastid parasites that primarily inflict skin leishmaniasis with transmission by sandfly vectors. Trypanosoma is responsible for African sleeping sickness and Chagas disease and is transmitted through tsetse flies and triatomine bugs respectively.
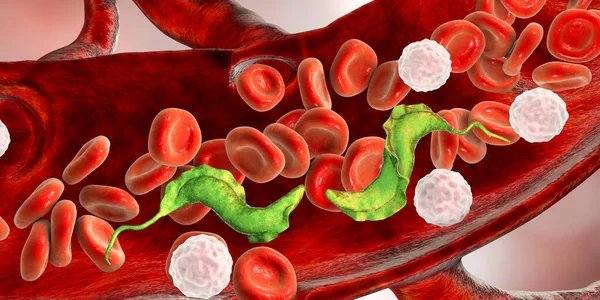
Leishmania exhibits amastigote and promastigote stages while Trypanosoma shows trypomastigote forms; both these parasites come with amastigote forms that need to develop further before reaching amastigotes or promastigote stages before infection becomes fatal.
Genetically, Leishmania displays diploidy with diverse genomes that alter drug resistance while Trypanosoma’s antigenic variation affects the immune response, complicating diagnosis via microscopy, PCR or serological tests.
Both infections may be severe with limited treatment options available and drug resistance concerns; thus understanding their individual differences is key to effective control, treatment, and prevention strategies.
What is Leishmania?

Leishmania refers to a protozoan parasite belonging to the family Trypanosomatidae that is responsible for leishmaniasis – an umbrella disease with symptoms spanning from skin infection, mucocutaneous, mucous membrane lesions, visceral involvement, and organ involvement that has infected millions in over 98 countries mainly located within tropical and subtropical climate zones.
Leishmania parasites possess an unusual lifecycle involving two main stages, extracellular promastigotes in their vector (sandfly) and intracellular amastigote stages within macrophages of host macrophages.
Transmission occurs when infected sandflies feed upon blood meals of their hosts and inject promastigotes which then become trapped inside these immune cells and transform into amastigotes which replicate within these immune cells.
Clinical manifestations of leishmaniasis vary based on the species of Leishmania involved, the immune response of its host, and which tissues it attacks. Cutaneous leishmaniasis typically presents with skin ulcers while visceral leishmaniasis affects internal organs leading to fever, weight loss, and other severe symptoms if left untreated.
Diagnosing parasitic infection generally involves identifying them through microscopy, PCR testing or serological methods, while treatment methods vary based on species and clinical form but usually includes antimonial compounds, amphotericin B, miltefosine or paromomycin as treatments, drug resistance has become an increasing threat.
Leishmania research centers around understanding its biology, genetic diversity, and host-parasite interactions; discovering novel therapies and vaccines as well as controlling transmission.
As leishmaniasis remains an intractable global health challenge, ongoing efforts must be taken to control transmission rates while improving diagnosis and treating methods; eventually lessening its burden and ultimately diminishing it altogether.
What is Trypanosoma?
Trypanosoma is a parasitic protozoa belonging to the family Trypanosomatidae that is responsible for several major human and animal illnesses, most notably African Trypanosomiasis (commonly referred to as Sleeping Sickness) and American Trypanosomiasis (Chagas Disease).
Trypanosoma parasites have an intricate lifecycle that typically involves both insect vectors and mammalian hosts, including tsetse flies for African trypanosomiasis and triatomine bugs for Chagas disease, to transmit parasites directly into hosts through blood meals.
Once inside, Trypanosoma species may undergo various developmental stages depending on their disease of infection from bloodstream trypomastigotes to intracellular amastigotes.
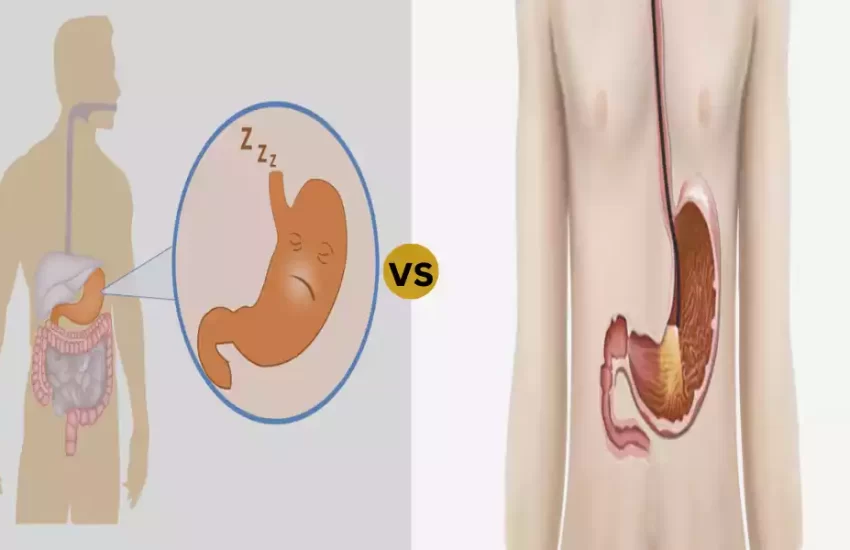
African trypanosomiasis affects humans and animals across sub-Saharan Africa, including humans and animals alike. The disease’s two primary forms are caused by two subspecies of Trypanosoma brucei: T. brucei gambiense and T. brucei rhodesiense. If left untreated, symptoms include sleep disruptions, confusion, and eventually coma.
Chagas disease, caused by Trypanosoma cruzi, is prevalent throughout Latin America and can result in cardiac and digestive complications.
Diagnosing Trypanosoma infections often involves microscopic examination of blood or tissue samples as well as molecular techniques like PCR and serological tests, among others.
Treatment depends on disease stage and severity; available drugs include suramin, pentamidine, melarsoprol, and nifurtimox. Unfortunately, drug resistance issues, limited treatment options, and difficulties managing disease make Trypanosoma an emerging global health threat.
Transmission and Distribution of Leishmaniasis and Trypanosomiasis
Transmission and Distribution of Leishmaniasis
Leishmaniasis is transmitted through bites from infected female sandflies of Phlebotomus (Old World) or Lutzomyia (New World), both belonging to the Phlebotomus genus; this cycle involves two main hosts: one being an insect vector host while the second host serves as a mammalian reservoir host. Sandflies gain parasites while taking blood meals from reservoir hosts that have been infected by parasites, which transform into infective promastigote forms that are then transmitted back out during subsequent blood meals to humans or other hosts.
Leishmaniasis is found throughout tropical and subtropical areas, with prevalence varying across Africa, Asia, the Middle East, Mediterranean countries and Central and South America. There are various cutaneous, mucocutaneous, and visceral forms of Leishmania responsible in various regions – each being caused by different species of Leishmania.
Transmission and Distribution of Trypanosomiasis
African Trypanosomiasis (Sleeping Sickness):
African trypanosomiasis is caused by Trypanosoma brucei parasites and spread via tsetse flies, with two subspecies, T. brucei gambiense and T. brucei rhodesiense, spreading from humans or animals into infected humans or animals before going back into both hosts again through complex transformation processes that take place within both hosts – affecting both host hosts over time as well as within.
Sub-Saharan Africa hosts this disease as T. brucei gambiense causes chronic forms while T. brucei rhodesiense causes acute forms. The latter species often causes chronic forms in West and Central Africa while T. brucei rhodesiense causes acute forms in East and Southern Africa respectively.
American Trypanosomiasis (Chagas Disease):
Chagas disease is caused by Trypanosoma cruzi and is typically transmitted through triatomine bugs, commonly referred to as kissing bugs. Once infected with parasites from infected sources such as humans, animals or reservoir hosts; their excrement then contaminates bite wounds or mucous membranes with infections leading to further spread.
Chagas is widespread across Latin America – particularly in rural and impoverished areas; transmission may occur via blood transfusions from the mother-to-child transmission as well as transmission through organ transplants as congenitally from mother-child transmission from the mother-child transmission as well as via blood transfusions from the mother-child transmission
During gestation and delivery from mother-child transmission from mother-child transmission of infection through organ transplants as well as congenitally from mother-child transmission through transmission during gestation from mother-child transmission during gestation.
Symptoms and Diagnosis of Leishmaniasis and Trypanosomiasis
Leishmaniasis Symptoms and Diagnosis:
SEVERAL CLINICAL FORMS (EACH WITH DIFFERENT SYMPTOMS):
Leishmaniasis may manifest in various clinical forms, each with different symptoms:
- Cutaneous Leishmaniasis: This form of the disease manifests with skin ulcers at the site of a sandfly bite. Although painless, healing time may be slow and leave scars. Swelling, inflammation, and sometimes fever may accompany these ulcers.
- Mucocutaneous Leishmaniasis: In addition to skin ulcers, this form can also lead to destructive lesions on the mucous membranes of the nose, mouth and throat causing significant disfigurement as well as functional and social impacts.
- Visceral Leishmaniasis (Kala-azar): This severe form affects internal organs like the spleen, liver and bone marrow and symptoms include prolonged fever, weight loss, fatigue anemia an enlarged abdomen due to an enlarged spleen and liver. If left untreated it could prove fatal.
Diagnose Leishmaniasis:
Diagnosing leishmaniasis involves multiple methods, including:
- Microscopic examination of stained tissue smears or biopsies to detect amastigotes within macrophages rov .
- PCR (Polymerase Chain Reaction) testing to detect Leishmania DNA.
- Serological tests such as the rK39 rapid diagnostic test that detect specific antibodies.
- Culture of parasites for species identification. Histopathological examination of biopsy samples.
Symptoms and Diagnosis of Trypanosomiasis:
Trypanosomiasis symptoms vary for African and American strains:
- African Trypanosomiasis (Sleeping Sickness): Early symptoms include fever, headaches, joint pain and itching. If left untreated it may progress into neurological symptoms including confusion, sleep disturbances and eventually coma.
- American Trypanosomiasis (Chagas Disease): An acute infection may cause fever, fatigue, body aches, and localized swelling at the site of infection (chagoma). Chronic infection can result in cardiac and gastrointestinal issues including heart rhythm disturbances or digestive issues.
Diagnosing Trypanosomiasis: (Learn more here) Diagnostic procedures may include:
- Microscopic examination of blood, lymph node aspirates or cerebrospinal fluid can detect parasites.
- serological tests can identify specific antibodies; while PCR allows the detection of parasite DNA.
- Xenodiagnosis involves allowing uninfected bugs to feed on a patient, and then inspecting these insects for signs of parasite presence.
- Cardiac assessment for Chagas disease-related cardiac issues.
Treatment Options for Leishmaniasis and Trypanosomiasis
Treatment Options for Leishmaniasis:
- Cutaneous Leishmaniasis: Small lesions may heal on their own, but larger or multiple lesions often require treatment. Cryotherapy or thermotherapy may be successful treatments while antimonials, amphotericin B, miltefosine and paromomycin can all provide systemic solutions.
- Mucocutaneous Leishmaniasis: Treatment usually involves taking antimonials, amphotericin B or miltefosine systemically for effective relief from lesions; multiple courses of therapy may be necessary in some cases.
- Visceral Leishmaniasis (Kala-azar): Treatment options include liposomal amphotericin B and miltefosine as first-line treatments; sodium stibogluconate and paromomycin may also be effective. If left untreated, Visceral Leishmaniasis could prove fatal; thus prompt medical intervention should be provided as soon as possible.
Trypanosomiasis Can Be Treated Effectively: What Are My Treatment Options:
- African Trypanosomiasis (Sleeping Sickness): Treatment depends on the stage of disease; early-stage infections typically respond well to treatments like pentamidine or suramin, while late-stage infections affecting the central nervous system typically need medications like melarsoprol or eflornithine which are toxic and difficult to administer.
- American Trypanosomiasis (Chagas Disease): Treatment for Chagas disease is most successful when administered during its acute stage. Nifurtimox and benznidazole are two effective antimicrobials used for this purpose, but outcomes in chronic stages tend to be less predictable; management primarily consists of relieving symptoms and avoiding complications.
Prevention Strategies for Leishmaniasis and Trypanosomiasis
Prevention Strategies for Leishmaniasis:
- Vector Control: Since sandflies are one of the primary vectors, effective measures must be taken to limit their population and prevent bites from them. These may include using insecticide-treated bed nets and screens as well as applying repellents directly onto exposed skin areas.
- Reservoir Host Control: Reducing contact between reservoir hosts such as rodents and humans can reduce transmission. This might involve improving sanitation, waste management and controlling population of potential hosts.
- Personal Protection: Wearing protective clothing during times of peak sandfly activity can help avoid bites.
- Environmental Controls: Altering the environment to decrease breeding sites for sandflies by clearing away debris or improving housing conditions can significantly decrease transmission risk.
- Vaccines: Studies to create effective vaccines against leishmaniasis continue, with some success being made against canine leishmaniasis in particular.
Prevention Strategies for Trypanosomiasis:
- Vector Control: Reducing transmission can be achieved by employing insecticide-treated traps, targets and livestock treatments to manage Tsetse fly populations.
- Animal Reservoir Management: Treating or culling reservoir hosts is an effective way to limit disease transmission between people and animals.
- Screening Donated Blood and Organs: Screening donations of blood and organs for Trypanosoma infections is essential in order to stop transmission through these routes.
- Avoid Tsetse Fly Infestation: Avoiding areas known for Tsetse fly infestation, particularly during times of high activity, can significantly decrease the risk of exposure.
- Treatment of Infected Individuals: Treating those who have become infected can prevent further disease progression and transmission.
- Vaccines and Research: While no widely available vaccine is currently available to prevent African and American trypanosomiasis, research is ongoing in order to develop vaccines against it.
Key Difference Between Leishmania and Trypanosoma
Here’s a simplified comparison chart between Leishmaniasis and Trypanosomiasis:
| Aspect | Leishmaniasis | Trypanosomiasis |
|---|---|---|
| Caused by | Leishmania parasites | Trypanosoma parasites |
| Transmitted by | Sandfly vectors (Phlebotomus and Lutzomyia) | Tsetse flies (African) and Triatomine bugs (American) |
| Clinical Forms | Cutaneous, mucocutaneous, visceral | African sleeping sickness, Chagas disease |
| Vectors | Sandflies | Tsetse flies (African), Triatomine bugs (American) |
| Life Cycle | Amastigote and promastigote stages | Trypomastigote and amastigote stages |
| Reservoir Hosts | Various mammals, rodents, dogs | Various mammals, rodents, domestic animals |
| Geographic Distribution | Global, tropical and subtropical regions | Africa (sleeping sickness), Latin America (Chagas) |
| Diagnosis Methods | Microscopy, PCR, serological tests, culture | Microscopy, PCR, serological tests |
| Symptoms in Humans | Skin ulcers, fever, organ damage (visceral) | Fever, neurological issues, heart problems |
| Treatment Options | Antimonials, amphotericin B, miltefosine, others | Pentamidine, suramin, melarsoprol, benznidazole, nifurtimox, eflornithine, others |
| Drug Resistance | Becoming a concern | Reported, especially in Chagas disease |
| Prevention | Vector control, personal protection, vaccines (ongoing research) | Vector control, animal reservoir control, screening, research |
| Impact on Health | Significant health burden, especially in endemic regions | Significant health burden in endemic regions |
| Research Focus | Development of vaccines, new treatments, vector control strategies | Vaccine development, new treatments, vector control strategies |
| Public Health Challenge | Neglected tropical disease, challenges in diagnosis and treatment | Neglected tropical disease, varying disease forms, limited awareness |
| Global Efforts | Various international organizations addressing prevention and control | Global partnerships, WHO and national efforts |
Conclusion
Leishmaniasis and Trypanosomiasis are parasitic diseases caused by different protozoan parasites transmitted via vectors like sandflies or tsetse flies that spread them throughout tropical regions, leading to various clinical forms, impacting millions and often leading to the diagnosis being complex; treatment options vary considerably, and prevention measures.
Typically includes vector control measures as well as protection and vaccine research efforts. Both diseases present public health challenges worldwide that require international efforts for greater management and control efforts.