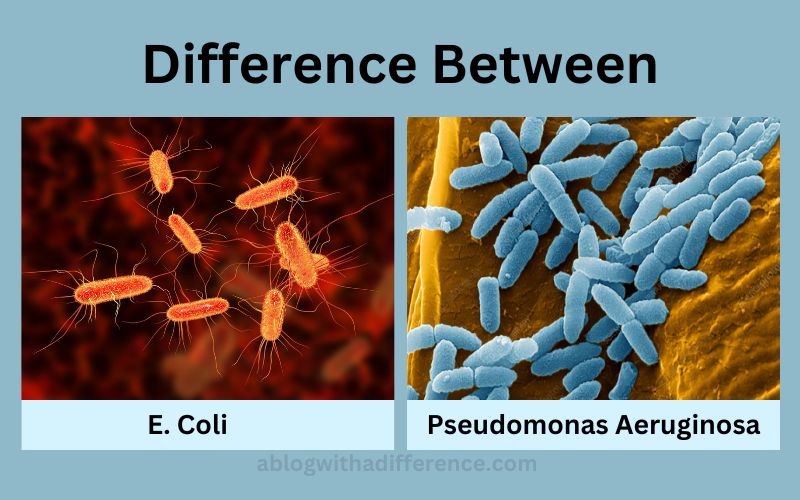
Difference Between E. Coli and Pseudomonas Aeruginosa
Brief explanation of E. coli and Pseudomonas Aeruginosa
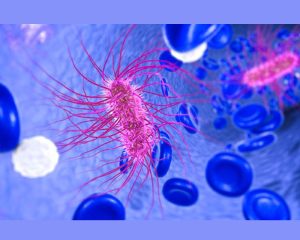
E. Coli (Escherichia Escherichia coli) bacteria are often found in the lower intestine and feces of warm-blooded mammals such as Humans. While most forms of E. bacteria do not pose serious threats, certain strains have the ability to cause urinary tract infections, foodborne illness, and sepsis which requires medical intervention for treatment.
Pseudomonas-aeruginosa infections can cause grave pneumonia, sepsis, and other severe illnesses in hospitals or healthcare environments where Pseudomonas-aeruginosa bacteria thrive, including soil, water, and other areas.
As this pathogen has an open-ended lifecycle it primarily attacks weak immune systems such as those who reside in hospitals or suffer from chronic illnesses requiring hospital care or those residing with weak immunity – such as patients in critical care units residing within healthcare environments.
Pseudomonas-aeruginosa can even spread between cells creating deadly infections which spread via airborne particles from the soil into medical environments where this pathogen thrives causing major health risks to occur resulting in hospital environments primarily.
Importance of understanding the difference between E. Coli and Pseudomonas Aeruginosa
Ascetic Scientists understand the distinctions between E. coli and Pseudomonas Aeruginosa are vitally important for several reasons:
1. Treatment and Diagnosis: Establishing the cause of infection is of vital importance when selecting appropriate antibiotic treatments; E. Pseudomonas aeruginosa infections may require different antibiotics; an incorrect diagnosis could lead to inadequate therapy or worsen the situation further.
2. Health and Safety: Both E. coli and Pseudomonas aeruginosa can pose Significant threats to public health leading to potentially life-threatening outbreaks that require researchers and public health experts to devise effective plans in order to stop or manage outbreaks. Being aware of their respective characteristics can assist researchers and public health specialists when devising prevention or response strategies to outbreaks.
3. Research: Studies on E. coli and Pseudomonas Aeruginosa that examine their physiological and genetic differences will enable researchers to develop effective new treatments and diagnostic tools for various infectious diseases, while simultaneously clarifying fundamental biological processes involved – further increasing our knowledge about microbiology.
What exactly is E. Coli?
It is a Gram-negative rod-shaped facultative anaerobic bacteria belonging to the Enterobacteriaceae family that most frequently occurs in lower intestinal environments of warm-blooded species. Though many strains exist today, E. Coli remains the predominant species for most intestinal bacteria colonization and colonisation of warm blooded species.
There have been reports of outbreaks resulting in E. Coli infection worldwide and several E. Coli strains exist within their populations as well.Coli strains typically do not present health threats and form part of normal microbiota in your gut, keeping the digestive tract functioning efficiently.
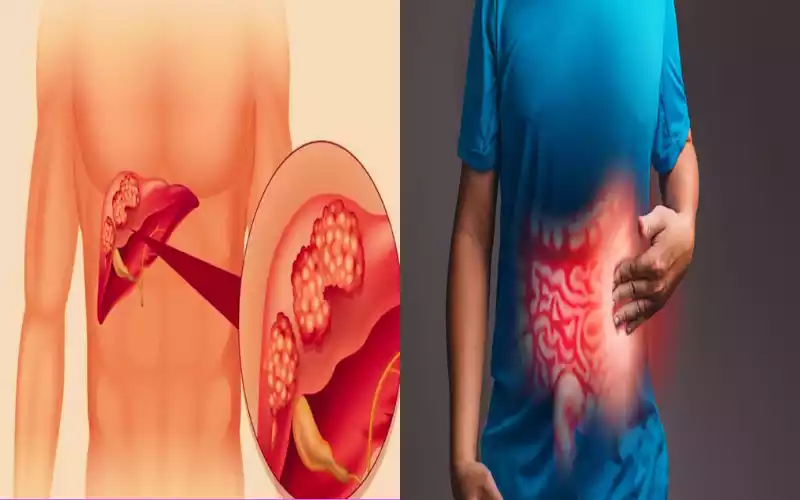
However, certain serotypes have the ability to cause food poisoning which results in abdominal cramping, diarrhea and vomiting symptoms.
E. O157:H7 produces Shiga toxin that causes severe food poisoning. E. Coli enters our system through oral routes through our faecal tract; common sources include raw vegetables, water sources and unpasteurized milk products containing E. Coli. However, proper food preparation and hygiene may reduce E. Coli-related illnesses significantly.
E. Coli is one of the primary prokaryotic model organisms used for studies involving recombinant DNA technology, making it a key player in many research endeavors.
Reasons behind choosing E. E. coli as the main model organism include its rapid expansion rate, access to low cost medium for growth manipulation of its environment as well as vast knowledge on its genomics and genetics.
What exactly is pseudomonas Aeruginosa?
Pseudomonas Aeruginosa (PAeruginosa), like E. coli, is an encapsulated bacteria with one flagellum. P. Aeruginosa can also be found as part of skin flora – though unknowingly becoming pathogenic; when found to be particularly aggressive it could cause cystic fibrosis, cancer, or burns if left to flourish uncontrolled.

P. aeruginosa stands out due to the fluorescent glow it produces when exposed to ultraviolet light, due to the production of fluorescent pigment pyoverdin by this bacteria.
Differences between E. coli and Pseudomonas Aeruginosa
Here are the main differences between E. coli and Pseudomonas Aeruginosa:
1. Location: E. coli usually inhabits the lower intestine of warm-blooded animals while Pseudomonas aeruginosa can be found everywhere from soil, to water sources, to various environments around a building or structure.
2. Oxygen requirements: E. coli is an anaerobe that requires oxygen in order to survive; Pseudomonas Aeruginosa on the other hand is considered an essential aerobe and requires it for growth.
3. Gram-staining: E. coli and Pseudomonas aeruginosa are both test positive, however, their identities can be distinguished through physical features like their morphologies.
4. Variability Factors and Disease Connections: When it comes to disease transmission, E. Coli and Pseudomonas aeruginosa bacteria both can play a significant role. Both strains have the capacity to cause infections as well as cause various illnesses;
E. coli typically results in urinary tract infection as well as foodborne illness outbreaks; while Pseudomonas aeruginosa strains often inflict infections upon people who lack immunity such as hospital patients who weakened immune systems – something E coli doesn’t.
5. Resistance to Antibiotics and Susceptibility to Them: Although both E. coli and Pseudomonas Aeruginosa possess the potential to become resistant to antibiotics Pseudomonas Aeruginosa stands out for being especially adept at developing immunity against various treatments for infections E. Coli often remains more vulnerable against various forms of antibiotics than its Pseudomonas aeruginosa counterpart.
Comparative Charts for E. Coli and Pseudomonas Aeruginosa
Here’s a chart that compares E. coli and Pseudomonas aeruginosa:
| Specific characteristics | E. coli | Pseudomonas aeruginosa |
|---|---|---|
| Habitat | Lower intestines of warm-blooded animals | Water, soil and various other environmental conditions |
| Oxygen requirements | Facultative anaerobe | Obligatory aerobe |
| Gram staining | Gram-negative | Gram-negative |
| Factors that influence the virulence | Fimbriae, adhesins, toxins, and fimbria | Exotoxin A, flagella LPS Proteases |
| Infections that are caused by | Foodborne illnesses | Infections are more likely to occur in people with weak immune systems, in particular the healthcare setting |
| Resistance to antibiotics | Can develop antibiotic resistance | The ability to become resistant to several antibiotics |
| Treatment | Typically, antibiotics are prescribed however, antibiotic resistance could be a cause for concern. | The treatment can be complicated due to resistance to antibiotics |
This chart outlines some of the major differences and commonalities in E. coli and Pseudomonas aeruginosa, such as their habitat oxygen requirements, virulence factors illnesses that cause them, antibiotic resistance and the treatment options.
Similarities between E. Coli and Pseudomonas Aeruginosa
E. coli and Pseudomonas Aeruginosa may differ in species but share certain commonalities here are just a few examples:
1. Gram-Negative Bacteria: Gram-negative bacteria: Both E. coli and Pseudomonas aeruginosa are Gram-negative bacteria, meaning that when stained Gram stains do not retain crystal violet staining.
2. Opportunistic Pathogens: E. coli is often mistakenly believed to be part of the regular gut flora; however, it’s an opportunistic pathogen capable of invading urinary tracts when introduced through urinary catheterization procedures and Pseudomonas aeruginosa has similar potential when introduced through weak immune systems.
3. Infections can cause illness: Both E. coli and pseudomonas aeruginosa can lead to infections in humans though each strain may lead to different diseases.
4. Antibiotic resistance: Both bacteria can develop Antibiotic resistance making infections more difficult to treat.
Even though E. coli and Pseudomonas aeruginosa share similarities, and understanding their distinction is key to being able to effectively treat infections caused by either bacteria.
Clinical significance of E. coli and Pseudomonas Aeruginosa
Both E. coli and Pseudomonas aeruginosa bacteria possess clinical relevance; both species can lead to various human infections that include:
1. E. coli: E. coli is one of the main sources of UTIs (Urinary Tract Infections) leading to foodborne illnesses such as diarrheal disease. Certain variants within EHEC such as enterohemorrhagic EHEC can even lead to kidney failure and severe diarrheal outbreaks.
2. Pseudomonas Aeruginosa: Pseudomonas Aeruginosa is an often prevalent pathogen capable of inflicting serious infections in individuals with compromised immune systems often linked with health-related problems like Bloodstream infections pneumonia and urinary tract infections as well as surgical wound infections.
Pseudomonas has become notoriously resistant to antibiotics over the years making treatment harder.
E. coli and Pseudomonas Aeruginosa both play an essential role in healthcare settings; their clinical relevance shows us the significance of timely identification, treatment, and prevention of infection in healthcare environments to stop the further spread of pathogens such as these bacteria.
Conclusion
E. coli and Pseudomonas Aeruginosa are two distinct bacteria with differing habitats species composition and clinical relevance. Understanding the key characteristics of both species is paramount in accurately diagnosing infections, selecting effective treatments, and devising preventive strategies against future outbreaks.
E. Coli is often associated with urinary tract issues as well as foodborne illnesses; Pseudomonas aeruginosa tends to target individuals who already have compromised immune systems – particularly within hospitals. Both bacteria can quickly develop resistance to antibiotics, making infection treatment harder than before.
Therefore, ongoing investigation of pathogens involved is required both to develop new treatments as well as combat antibiotic-resistant strains from spreading further.