10 Ways Difference Between Colitis and Proctitis Can Help You Live long time
Brief Overview of Colitis and Proctitis
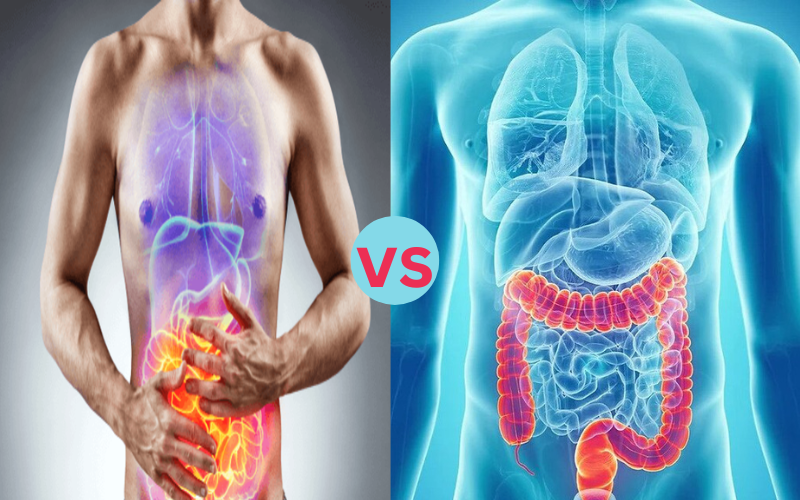
Colitis and proctitis are two inflammatory digestive conditions, each targeting its respective parts. Colitis affects inflammation of the colon’s lining, leading to symptoms like abdominal pain and diarrhea; proctitis targets rectal tissue instead.
Colitis refers to inflammation of the colon, commonly seen in conditions like ulcerative colitis or Crohn’s disease. Proctitis involves localized inflammation limited to just the rectum, leading to symptoms like rectal bleeding or pain; differentiating between these conditions for accurate diagnosis and tailor-made treatment strategies is key.
what is Colitis?
Colitis, in medical parlance, refers to inflammation of the colon. This part of the large intestine plays an integral part in digesting food and absorbing water and electrolytes from digested material, and inflammation due to various sources may include ulcerative colitis or Crohn’s disease, infections, ischemia or microscopic colitis.
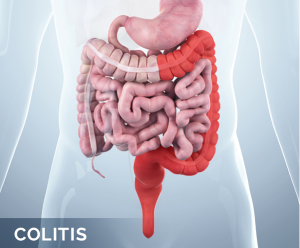
Ulcerative colitis primarily targets the inner lining of the colon and leads to ulcers and chronic inflammation that results in ulcers. It often presents with symptoms including abdominal pain, diarrhea, rectal bleeding, and weight loss. Crohn’s disease, another form of colitis that impacts any part of your digestive tract resulting in deep-seated inflammation that reaches into each bowel wall lining, also falls under this classification.
Diagnosing colitis involves reviewing medical history information, conducting physical exams, performing endoscopic procedures and biopsies as part of its diagnosis, treating medications to suppress inflammation or modify immunity or lifestyle adjustments and diet modifications; or in severe cases or when complications develop surgery might also be considered to remove affected portions from the colon.
what is Proctitis?
Proctitis refers to inflammation of the rectal lining, located near the anus. It may result from infections (sexually transmitted diseases and bacteria infections) as well as from inflammation caused by chronic diseases (particularly when limited to just the rectum), radiation therapy treatments or even autoimmune conditions like ulcerative colitis.

Common symptoms of proctitis can include rectal pain, discomfort, bleeding, and the frequent urge for bowel movement. Systemic symptoms like fever and fatigue may also accompany it; diagnosis requires physical examination, endoscopic procedures, and biopsies in order to identify both the cause and extent of inflammation.
Treatment for proctitis depends on its cause mild cases caused by infections may require antibiotics and antiviral medicines for more inflammatory causes, topical or oral anti-inflammatory medication could provide relief; lifestyle modifications including diet changes or stress reduction could also aid in lessening discomfort. Therefore, early diagnosis and management are vital in order to protect rectal health.
Symptoms of Colitis and Proctitis
Colitis refers to inflammation of the colon. Symptoms may include abdominal cramping accompanied by persistent diarrhea that might even contain blood. People suffering from colitis may feel an urgent urge to move their bowels often leading to distressful urgency weight loss and fatigue may result from inflamed tissue within the colon reducing absorption of nutrients from food sources and potentially perforation or toxic megacolon, or an increased risk for colorectal cancer in severe cases.
Proctitis refers to inflammation localized within the rectum, with symptoms consisting of rectal discomfort. People suffering from proctitis often report rectal pain that resembles constant ache or sharp sensation, and rectal bleeding that leaves bright red blood-streaked stool behind; inflammation may cause fullness or sensations that one needs to pass stool even though one has done so already.
Although systemic symptoms associated with proctitis tend to be milder compared with more extensive colitis conditions such as fever fatigue weight loss might still occur alongside this condition.
What are the causes of Colitis and Proctitis
Colitis Causes:
Colitis may have various root causes. Irritable Bowel Disorder (IBD), including ulcerative colitis and Crohn’s disease, are leading contributors, with their abnormal immune responses targeting the colon’s lining. Bacterial or viral infections often trigger colitis by infiltrating food or water supply sources or through foodborne contaminants reduced blood flow due to blood clots or narrowed arteries can result in reduced oxygen availability for colonic circulation.
Microscopic colitis with chronic watery diarrhea is related to immune dysfunction with collagenous or lymphocytic colitis being subtypes within microscopic colitis itself resulting from disruption within its immune system.
Dysfunctional mechanism with collagenous and lymphocytic subtypes making up microscopic colitis symptoms associated with immune dysfunctional pathways leading back into its respective organs for proper distribution into its natural environment.
Proctitis Causes:
Proctitis can be caused by any factor which directly impacts on the rectal area. Sexually transmitted infections like gonorrhea, chlamydia, and herpes have all been implicated as potential sources. Ulcerative colitis and Crohn’s disease that only involves the rectum can also trigger proctitis while radiation therapy used for cancer treatments could contribute.
Autoimmune diseases as well as infections from nonsexually transmitted sources and certain medications could all also trigger proctitis symptoms so it’s imperative that its causes be identified so that appropriate treatment strategies can be implemented successfully.
Diagnosis Method of Colitis and Proctitis
Diagnostic Approach of Colitis:
Diagnosing colitis requires taking an in-depth approach, to ascertain both its source and scope of inflammation. Physicians usually begin with an extensive medical history review and physical exam that covers symptoms, family history, and overall health.
Laboratory tests (such as blood tests to measure inflammation markers), and endoscopic procedures like colonoscopy or sigmoidoscopy allow direct visualization of the colon interior, permitting biopsies for histopathological analysis that help differentiate among various forms of colitis as well as rule out other conditions
Proctitis Diagnosis:
Rectal inflammation must be assessed accurately to accurately pinpoint possible sources. A digital rectal exam is often utilized in diagnosing proctitis. An endoscopic procedure like proctoscopy provides visual access to the interior rectum for biopsies.
while laboratory cultures or polymerase chain reaction tests (PCR tests) help detect infectious causes, particularly sexually transmitted proctitis cases lab cultures or PCR. Finally, medical imaging such as MRI, CT scans might help evaluate the extent of inflammation while ruling out other conditions that might also exist.
What is the treatment for Colitis and Proctitis?
Treatment Options for Colitis:
Medications:
- Medication (Anti-inflammatories, corticosteroids and immunomodulators) can be taken to control inflammation and symptoms; such as aminosalicylates, corticosteroids or immunomodulators.
- Biologic therapies which target specific proteins involved with inflammation may also help in severe cases.
- If bacterial infection is the source, antibiotics may be prescribed.
Lifestyle Modifications:
- Dietary adjustments could include avoiding trigger foods and keeping hydrated by following a balanced diet with adequate water intake.
- Prolonged anxiety and tension can aggravate symptoms, so relaxation techniques and coping strategies should be employed as soon as possible to ease pressure.
Surgery:
- For cases in which medications fail or complications develop, surgery might be required in severe instances to remove affected portions of colon. Regular
Monitoring:
- To stay healthy it’s essential that ongoing monitoring be maintained.
Treatment of Proctitis:
Topical Medications:
- Routine checkups to monitor disease progression, adjust medications accordingly and manage flare-ups effectively are key elements in effective Proctitis care.
- Topical medications for Proctitis may include rectal suppositories or creams containing anti-inflammatory agents designed specifically to target rectal inflammation.
- Alternatively orally administered anti-inflammatories may also help. Oral medicines also offer relief of rectal discomfort.
Oral Medications:
- Oral anti-inflammatory medicines such as aminosalicylates or corticosteroids might be prescribed to address more extensive inflammation.
Underlying Cause Treatment:
- Addressing infections with appropriate antibiotics or antiviral medicines as needed.
Diet and Lifestyle Considerations:
- Dietary changes that reduce symptoms, like eliminating spicy or irritating foods and practicing stress management are integral.
Supportive Care:
- Supportive Care includes using soothing ointments for comforting effects as well as practicing good hygiene in the rectal area, with regular follow-up and follow-through checks scheduled as part of care plans.
Regular Follow-Up:
- Regular appointments with healthcare providers to monitor progress, adjust treatment as necessary and identify and prevent complications are crucial in keeping patient well-being at top form.
When is surgery needed for colitis Colitis and Proctitis?
Surgery plays a vital role in treating colitis and proctitis when other treatments prove insufficient. In cases of severe colitis where medical therapies fail or complications like perforation or excessive bleeding arise, surgical removal of the affected section could be required to improve quality of life and avoid future complications. Proctitis surgery should also be considered when the inflammation becomes extensive and causes discomfort or bleeding, or does not respond to medical treatments.
Surgery options range from partial colectomy, where only affected colon segments are removed, to more extensive procedures like total proctocolectomy involving creating a stoma and often creating an end ileostomy stoma. Working closely with medical professionals allows individuals to make well-informed decisions regarding surgery and post-op care.
Colitis vs. Proctitis: Key Differences
Here’s a simple comparison chart outlining key differences between colitis and proctitis:
| Aspect | Colitis | Proctitis |
|---|---|---|
| Definition | Inflammation of the colon’s lining | Inflammation of the rectal lining |
| Location | Throughout the colon | Limited to the rectum |
| Symptoms | Abdominal pain, diarrhea, rectal bleeding | Rectal pain, bleeding, urgency |
| Extent of Inflammation | Can affect the entire colon or specific segments | Confined to the rectal area |
| Causes | Infections, IBD, ischemia, autoimmune disorders | Infections, IBD, radiation, autoimmunity |
| Diagnostic Procedures | Colonoscopy, biopsies, endoscopy | Proctoscopy, biopsies, digital examination |
| Treatment | Medications, lifestyle changes, surgery | Topical medications, oral meds, lifestyle |
| Complications | Perforation, toxic megacolon, cancer risk | Chronic discomfort, bleeding, infections |
| Surgical Options | Colectomy, ileostomy, colostomy | Proctectomy, coloanal anastomosis, stoma |
| Impact on Lifestyle | Variable based on severity and treatments | Generally less extensive than colitis |
What are the Similarities Between Colitis and Proctitis?
Colitis and proctitis share similar inflammatory digestive conditions that impact multiple anatomical regions within the digestive tract, though their causes vary considerably. Both conditions may result from factors like infections, immune reactions or chronic illnesses underlying them causing inflammation that manifests differently depending on which organ system it affects.
Both conditions may lead to discomfort and bleeding in various places throughout your body, with symptoms typically linked to their affected location for instance abdominal pain and diarrhea in colitis and rectal discomfort with proctitis respectively. Diagnosing colitis and proctitis involves reviewing medical history information, and performing physical exams, endoscopic procedures, and biopsies.
Treatment approaches vary based on inflammation levels but typically consist of medications, lifestyle modifications, and surgery in more serious instances. Early identification and management is key in order to avoid complications, manage symptoms effectively, and increase the quality of life for affected individuals.
How do you prevent Colitis and Proctitis?
Preventing colitis and proctitis requires adopting a healthy lifestyle, managing any underlying medical conditions effectively, and practicing appropriate hygiene. Though some causes, such as autoimmune disorders, are difficult to prevent entirely, certain measures may help lower their risks or severity. A diet rich in fiber and nutrients could support overall gut health thereby potentially decreasing inflammation risks and the chance for disease outbreaks.
Substitution of nonsteroidal anti-inflammatory drugs (NSAIDs) with antibiotics when not medically necessary is one way of combatting irritation-induced inflammation. Maintaining a healthy weight and managing stress through physical exercise, relaxation techniques, and adequate rest can lower the risk of inflammation exacerbation.
Also practicing safe sex using protection can minimize any chance of sexually transmitted infections that might lead to proctitis. Regular check-ups with healthcare providers are key in identifying risk factors early and designing tailored preventive strategies tailored specifically for each person’s unique health profile.
What is the best diet for proctitis?
Diet for proctitis should focus on relieving irritation and inflammation of the rectal lining while catering to individual preferences and tolerance.
Here are dietary suggestions that could assist in treating proctitis:
- Low-Fiber Foods: When experiencing flare-ups, choose low-fiber foods like well-cooked vegetables, white rice, and lean proteins to ease discomfort in your digestive tract. This may reduce irritation.
- Avoid Trigger Foods: Identify and avoid foods that trigger symptoms, such as spicy foods, caffeine beverages, alcoholic beverages and highly processed products. Common triggers could include spicy meals, coffee beverages or alcohol beverages as well as highly processed snacks and meals.
- Hydrate regularly: Drink plenty of water throughout the day in order to remain properly hydrated if diarrhea is an issue.
- Probiotics: Eating foods rich in probiotics such as yogurt or fermented foods is one way to support digestive health and ensure optimal gut wellbeing.
- Soft Foods: For optimal digestion, choose foods like cooked fruits, plain pasta and well-prepared oatmeal that can easily be digested.
- Foods Rich in Anti-Inflammatory Properties: For anti-inflammatory effects, consume foods such as salmon or mackerel as well as leafy greens and berries, to support wellness.
- Aloe Vera Juice: Some individuals find comfort by drinking aloe vera juice, which may offer anti-inflammatory benefits.
- Herbal Teas: Chamomile, ginger and peppermint teas may provide soothing effects for digestive health.
- Cooking Methods: For better digestive health, select cooking methods like steaming, baking or grilling over frying. These processes tend to be gentler on your digestive tract.
- Consume Small Meals Frequent: Eating small meals frequently and regularly can help your digestive process run more smoothly and minimize discomfort.
Conclusion
Colitis and proctitis are two inflammatory digestive conditions, each targeting its respective parts. Colitis affects inflammation of the colon’s lining, leading to symptoms like abdominal pain and diarrhea; proctitis targets rectal tissue instead.
Diagnosis includes exams, endoscopies, biopsies as well as biopsies; treatment approaches depend on inflammation levels as well as any underlying causes; such treatments might include medications, lifestyle modifications or surgical solutions based on individual need; early identification is critical in terms of both conditions’ results for individuals affected.