CAR-T and TCR-T 12 solid and best difference don’t you know
CAR-T and TCR-T therapies. Both therapies leverage the immune system’s capacity to destroy and target cancerous cells – offering promising new approaches against this scourge.
Definition of CAR-T cell therapy
CAR-T therapy (Chimeric Antigen Receptor T Cell Therapy) is an immunotherapeutic strategy to combat certain cancer types. The technique works by reprogramming T-cells – immune cells responsible for attacking foreign or abnormal cells – into cancer-targeting T cells by genetically modifying them so they express a CAR on their surface.
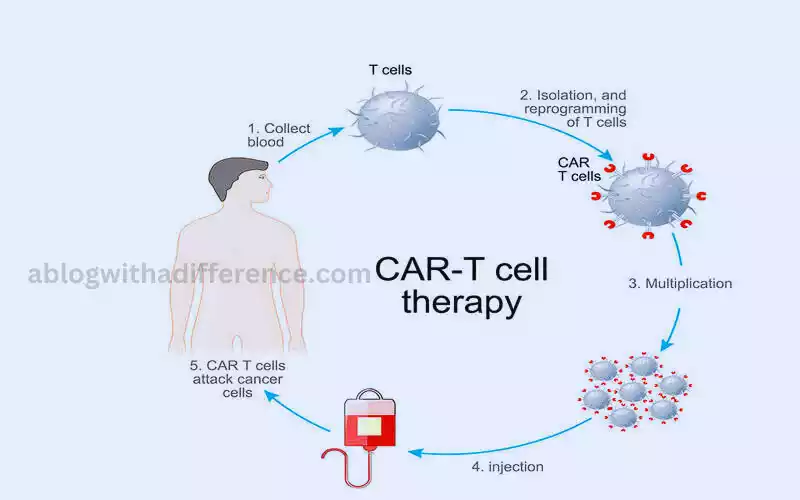
CARs are artificial receptors composed of an antigen-binding domain derived from antibodies and signaling components derived from T cells. This combination allows CAR-T cells to recognize specific antigens found on cancer cell surfaces and bind them, activating T-cells into proliferative responses against them through signaling components derived from T-cells.
Once modified, CAR-T cells are expanded in the laboratory before being reinfused into the patient’s bloodstream. Once in their new home, these CAR-T cells continue to multiply and search out cancerous cells expressing the targeted antigen; upon encountering any, they mount an effective attack, effectively wiping them out.
CAR-T cells have shown great promise in treating hematologic cancers such as acute leukemia and non-Hodgkin’s lymphoma despite other therapies have failed. It marks an innovative breakthrough in cancer therapy with the potential to revolutionize how certain cancer types are addressed, giving hope to those previously incurable of disease.
Definition of TCR-T cell therapy
TCR-T Cell Therapy, also referred to as T-Cell Receptor T Cell Therapy (TCRTC), utilizes TCRs – or T cell receptors – as part of its arsenal in fighting cancer cells. CAR-T is another immunotherapy option which employs patient’s immune cells in an attempt to attack cancerous ones. CCR-T is similar but operates more slowly.
TCR-T cells are increasingly being employed in cancer therapy as an alternative to CARs (chimeric antigen-receptors) that recognize cancerous cells. T cells modified with T cell receptor (TCR) expression enable TCRs on T-cell surfaces to recognize antigens on target cells such as cancer cells.
TCR-T Cell Therapy involves isolating T-cells from within a patient, selecting those equipped with TCRs able to recognize cancer-specific antigens and genetically modifying them for enhanced anticancer activity in a lab setting, then infusing those modified TCRs back into his or her bloodstream for therapeutic effect.
Once inside of a patient, TCR-T cells search for cancerous cells displaying antigens they target, activating when they encounter these cancer cells which then induce an immune response and destroy these cancerous cells.
TCR-T therapy allows cancer specialists to target cancer-specific antigens within cells – including intracellular ones which CAR-T cells cannot access – for treatment purposes, making TCR-T an ideal therapy choice against solid tumors as well as hematologic cancers.
TCR-T Cell Therapy shows promise, yet is in its early stages compared to CAR T cell therapy. Current trials and studies aim to optimize its safety, efficacy and feasibility.
Rise of immunotherapy in cancer treatment
The rise of immunotherapy in cancer treatment marks a transformative shift in the approach to fighting cancer. Immunotherapy uses immunology to attack cancer cells more precisely and safely, providing a less toxic, targeted alternative to chemotherapy or radiation treatments. Immunotherapy research is still in its infancy but has proven remarkably successful against all forms of cancers.
Below are a few factors which have contributed to immunotherapy’s rise as an option:
- Advancements in Understanding the Immune System: Understanding the complex interactions among cancer cells, immune cells and immunity has resulted in significant advances in developing immunotherapies. Scientists gained insight into how cancerous cells evade immune reactions and identified possible intervention targets.
- Breakthroughs in Immunotherapy: Recent advances in immunotherapy such as CAR-T cells, TCR T cell therapy, cancer vaccinations and immune-modulating drugs have dramatically expanded patients’ treatment options for cancer. Clinical studies have confirmed their efficacy against numerous forms of cancers; as are approvals.
- Success in Clinical Trials: Positive results from early clinical trials have demonstrated the potential of immunotherapy in achieving durable responses and even complete remissions in patients with advanced or metastatic cancers. These successes have driven further research and investment in the field.
- FDA Approvals and Expanded Indications: The U.S. Food and Drug Administration and various regulatory authorities worldwide have approved immunotherapies as treatment options for various forms of cancer. Some therapies have received expanded indications, allowing their use in multiple cancer settings.
- Personalized Medicine and Biomarkers: Immunotherapy has shown significant benefits in certain patient populations, leading to the concept of personalized medicine. Biomarkers can be used to predict which patients are likely to respond well to immunotherapies, thereby optimizing treatment results while decreasing adverse side effects.
- Combination Therapies: Researchers are exploring combinations of different immunotherapies and their integration with traditional treatments to enhance effectiveness. Combinations with targeted therapies, chemotherapy, or radiation therapy have shown synergistic effects, improving overall treatment responses.
- Improved Safety Profiles: Immunotherapies often have different side effect profiles compared to conventional treatments. They may still cause adverse immune events. These treatments tend to be better tolerated by patients during therapy resulting in improved quality of living during therapy.
- Long-Term Benefits: Some immunotherapies have shown the potential for durable responses, leading to long-term survival and even potential cures in specific cancer types. These outcomes were previously rare with traditional treatments.
The rise of immunotherapy in cancer treatment has transformed the landscape of oncology, offering new hope to patients with previously limited treatment options. Immunotherapy will likely play an increasing role in cancer treatments as research expands and our knowledge about cancer and immune systems deepen.
Mechanisms of Action
The Mechanisms of action for immunotherapies, particularly CAR-T cell therapy and TCR-T cell therapy, as well as checkpoint inhibitors, play crucial roles in their effectiveness in treating cancer. Each therapy employs distinct mechanisms to target and eliminate cancer cells, enhancing the body’s immune response.
Let’s explore the mechanisms of action for these immunotherapies:
- CAR-T Cell Therapy:
- Collection of T-cells: T-cells are extracted from the patient’s blood through leukapheresis.
- Genetic Modification: The collected T-cells are genetically engineered to express a chimeric antigen receptor (CAR) on their surface.
- Antigen Recognition: The CAR is designed to recognize specific tumor-associated antigens present on cancer cells.
- T-cell Activation: When the CAR-T cells encounter cancer cells expressing the targeted antigen, the CAR binding triggers T-cell activation.
- Immune Response: Activated CAR-T cells rapidly multiply and launch a robust immune response against the cancer cells, leading to their destruction.
- Persistence: Some CAR-T cells persist in the patient’s body, offering long-term surveillance against potential cancer recurrence.
- TCR-T Cell Therapy:
- T-cell Isolation: T-cells are obtained from the patient’s blood.
- TCR Selection: T-cells expressing naturally occurring T-cell receptors (TCRs) with specificity for cancer-specific antigens are selected.
- Genetic Modification: The selected T-cells are genetically modified to enhance their anti-cancer activity and proliferation.
- Antigen Recognition: The modified TCRs enable T-cells to recognize specific cancer antigens presented by major histocompatibility complex (MHC) molecules on the surface of cancer cells.
- T-cell Activation: Upon recognizing the cancer-specific antigen, the TCR-T cells are activated to initiate an immune response against the cancer cells.
- Immune Response: Activated TCR-T cells proliferate and target cancer cells expressing the specific antigen, leading to tumor cell destruction.
- Checkpoint Inhibitors:
- Immune Checkpoint Blockade: Checkpoint inhibitors are monoclonal antibodies that block inhibitory immune checkpoints, such as PD-1/PD-L1 and CTLA-4, which prevent excessive immune activation.
- T-cell Activation: By blocking these checkpoints, checkpoint inhibitors enhance the activation of T-cells, allowing them to mount a stronger immune response against cancer cells.
- Reinvigorating Immune Response: Checkpoint inhibitors “reinvigorate” exhausted T-cells, which have become less effective in recognizing and attacking cancer cells.
- Proliferation: The activated T-cells can then proliferate and effectively target cancer cells throughout the body.
- Long-Term Memory: Some T-cells may form memory cells, providing long-term immunity against cancer cells.
These immunotherapies all work to enhance the body’s immune system’s ability to recognize and destroy cancer cells. By leveraging different mechanisms of action, they offer promising treatment options for various types of cancer, often providing durable responses and improved patient outcomes.
Antigen Specificity
Antigen specificity is a critical aspect of immunotherapy that ensures targeted and precise recognition of cancer cells by the immune system. Immunotherapies based on CAR T cells or TCR T cells must recognize and bind specific antigens on cancerous cells to be effective. Otherwise they cannot distinguish between healthy cells and cancerous ones.
It’s therefore crucial that immunotherapies can identify specific antigens on cancer cell surfaces to distinguish between healthy and cancerous ones.
- CAR-T Cell Therapy:
- CAR Design: Chimeric antigen receptors (CARs) used in CAR-T cell therapy are designed to recognize specific tumor-associated antigens (TAAs) on cancer cells.
- Antigen Selection: The choice of the antigen targeted by the CAR is crucial, as it determines which cancer cells the CAR-T cells will attack.
- Broad Antigen Recognition: CAR-T cells can recognize a wide range of antigens, including surface proteins expressed on various cancer types.
- TCR-T Cell Therapy:
- TCR Specificity: T-cell receptors (TCRs) used in TCR-T cell therapy are naturally occurring and have specificity for specific antigen peptides presented by major histocompatibility complex (MHC) molecules on the surface of cells.
- Intracellular Antigens: TCRs enable T-cells to recognize antigens from inside cancer cells, including those derived from mutated or abnormal proteins.
- Checkpoint Inhibitors:
- Inhibitory Checkpoint Blockade: Checkpoint inhibitors target specific inhibitory immune checkpoints, such as PD-1/PD-L1 and CTLA-4, that limit T-cell activity against cancer cells.
- Restoring T-cell Specificity: By blocking these checkpoints, checkpoint inhibitors restore the specificity of T-cell recognition and activation against cancer cells.
Antigen specificity is crucial to prevent off-target effects and immune responses against healthy tissues. While CAR-T cell therapy and TCR-T cell therapy can be designed to target specific cancer antigens, checkpoint inhibitors work by unleashing the body’s existing T-cells against cancer cells, restoring their specificity without genetic modification.
Determining the appropriate antigen target is a significant consideration in the development of immunotherapies. The choice of antigen can impact the effectiveness of the treatment, as some antigens may be more prevalent or critical for cancer cell survival than others. Additionally, the heterogeneity of cancer cells within a tumor and between patients can pose challenges in identifying suitable antigens for immunotherapies.
Antigen specificity is a fundamental concept in immunotherapy, allowing for selective recognition and targeting of cancer cells while sparing healthy tissues, ultimately leading to improved therapeutic outcomes and reduced side effects.
Clinical Applications
Immunotherapy has shown great promise as an approach for the treatment of various cancer types, such as CAR-T cells, TCR T cell therapy and checkpoint inhibitors. With ongoing research efforts and more clinical trials being completed, immunotherapies continue to expand their scope in clinical applications.
Below are some notable clinical applications of immunotherapies:
1. CAR-T Cell Therapy:
- Acute Lymphoblastic Leukemia (ALL): CAR-T therapy has proven highly successful at treating ALL in young adults and children who have relapsed, especially among younger age groups.
- Non-Hodgkin Lymphoma: CAR T cell therapy has proven itself effective against certain subtypes of this cancer, such as diffuse large B cells lymphoma and primary mediastinal B cells lymphoma.
- Multiple Myeloma: Ongoing clinical trials are evaluating the use of CAR-T cell therapy for multiple myeloma, a type of blood cancer.
2. TCR-T Cell Therapy:
- Solid Tumors: TCR-T cell therapy holds potential in targeting solid tumors, including melanoma, ovarian cancer, lung cancer,
- Hematologic Malignancies: TCR-T cell therapy is being explored for various hematologic malignancies, expanding its application beyond CAR-T therapy.
3. Checkpoint Inhibitors:
- Melanoma: Some patients have experienced long-term and durable benefits from anti-PD-1 antibodies.
- Lung Cancer: Checkpoint inhibitors showed significantly improved outcomes when used both alone and with chemotherapy for non-small cell lung carcinoma (NSCLC).
- Renal Cell Carcinoma: Checkpoint inhibitors have demonstrated efficacy in treating advanced renal cell carcinoma, offering an alternative to traditional therapies.
- Bladder Cancer: Checkpoint inhibitors have shown promising results in advanced or metastatic bladder cancer patients, improving response rates and survival.
4. Combination Therapies:
- Improved Outcomes: Combining immunotherapies with each other or with traditional treatments like chemotherapy or radiation therapy can lead to enhanced treatment responses and improved survival rates.
- Overcoming Resistance: Combination therapies aim to overcome mechanisms of resistance that cancer cells may develop against single-agent immunotherapies.
5. Potential for Cure:
- In certain cases, immunotherapies, especially CAR-T cell therapy, have achieved long-term remissions and even cures in patients with otherwise treatment-refractory or terminal cancers.
Immunotherapies have proven successful against some cancers and patients; however, not everyone responds the same. Biomarkers and patient characteristics are being identified to predict response and guide personalized immunotherapy treatment plans. Clinical applications continue to expand and research is taking place that could potentially benefit more cancer patients in the future.
Safety Considerations
Immunotherapies must be designed and applied with care to avoid potential risks to patient safety. While these treatments have shown remarkable efficacy, they can also lead to potentially severe side effects, particularly immune-related adverse events (irAEs). Understanding and managing these safety concerns are essential for ensuring the well-being of patients undergoing immunotherapy.
Below are some key safety considerations for CAR-T cell therapy, TCR-T cell therapy, and checkpoint inhibitors:
1. CAR-T Cell Therapy:
- Cytokine Release Syndrome (CRS): CRS is a severe systemic inflammatory response caused by the rapid and massive release of cytokines from activated CAR-T cells.In extreme instances, it may lead to organ dysfunction, fever, hypotension and even death.
- Neurological Toxicity: Also referred to as CAR cell-related Encephalopathy Syndrome (CRES), neurological toxicities may manifest themselves through confusion, delirium or seizures. Although its exact mechanisms remain ununderstood, researchers believe they might be due to inflammation caused by cytokine proteins in the brain.
- Tumor Lysis Syndrome (TLS): Rapid destruction of cancer cells can lead to the release of intracellular contents into the bloodstream, causing metabolic disturbances and potential organ damage.
2. TCR-T Cell Therapy:
- Off-Target Effects: TCR-T cell therapy can inadvertently target normal tissues expressing the targeted antigen, leading to unintended toxicity.
- Cytokine Release: TCR-T cell activation can trigger a cytokine release similar to CRS, causing systemic inflammation and potential adverse effects.
3. Checkpoint Inhibitors:
- Immune-Related Adverse Events (irAEs): Checkpoint inhibitors can lead to irAEs affecting various organs due to the unleashed immune response against healthy tissues. Common irAEs include dermatitis, colitis, pneumonitis, and endocrine dysfunction.
- Autoimmune Reactions: Checkpoint inhibitors can exacerbate pre-existing autoimmune conditions or lead to the development of new autoimmune disorders.
4. Management and Mitigation:
- Patient Selection: By carefully considering disease characteristics, health status and any possible risk factors when selecting patients for immunotherapy treatment, one can more accurately anticipate which individuals would most benefit while simultaneously mitigating risks.
- Monitoring: Close monitoring of patients during and after treatment is crucial to detect and manage adverse events promptly.
- Grading and Management Guidelines: Standardized grading and management guidelines for adverse events help healthcare providers assess the severity of toxicities and guide appropriate interventions.
- Supportive Care: Supportive care measures, such as anti-inflammatory drugs, immune-modulating therapies, and appropriate organ-specific interventions, can help manage irAEs effectively.
5. Ongoing Research:
- Predictive Biomarkers: Predictive biomarkers can assist physicians in selecting patients most likely to respond positively to immunotherapy and assess any risks for potential side effects.
- Combinatorial Approaches: Combining immunotherapies with other treatments aims to enhance efficacy while managing toxicities.
While safety should always come first, immunotherapies may prove more advantageous in many instances than any potential risks they present; especially when other treatment alternatives have proven ineffective. Rigorous safety monitoring, proper patient selection, and improved management strategies continue to advance the field of immunotherapy, making these treatments safer and more effective for cancer patients.
Manufacturing Process
Manufacturing immunotherapies is an intricate and detailed process. CAR-T and TCR T cell therapies both demand precise work in order to provide safe and effective treatments.
Here is an overview of how immunotherapy products are manufactured:
1. CAR-T Cell Therapy Manufacturing Process:
- Patient Leukapheresis: The process begins with the collection of peripheral blood from the patient through leukapheresis. Leukapheresis is a procedure that separates and collects white blood cells, including T-cells, from the patient’s blood.
- Isolation and Activation of T-cells: T-cells are isolated from the collected leukapheresis product using specialized laboratory techniques. The isolated T-cells are then activated using specific stimulatory signals to prepare them for genetic modification.
- Genetic Engineering: The activated T-cells undergo genetic engineering to introduce the CAR gene into their genome. The CAR is designed to target specific tumor-associated antigens on cancer cells.
- Ex Vivo Expansion: The genetically modified T-cells are cultured and allowed to expand in the laboratory. This step is essential to generate a sufficient number of CAR-T cells for therapeutic use.
- Quality Control: Throughout the manufacturing process, strict quality control measures are implemented to ensure that the final CAR-T cell product meets safety and efficacy standards. This includes testing for the presence of CAR on T-cells and evaluating their potency.
- Cryopreservation: Once the CAR-T cell product meets quality control requirements, it is cryopreserved (frozen) to maintain its viability during transportation to the treatment site.
- Infusion: The cryopreserved CAR-T cell product is thawed and then infused back into the patient through intravenous administration.
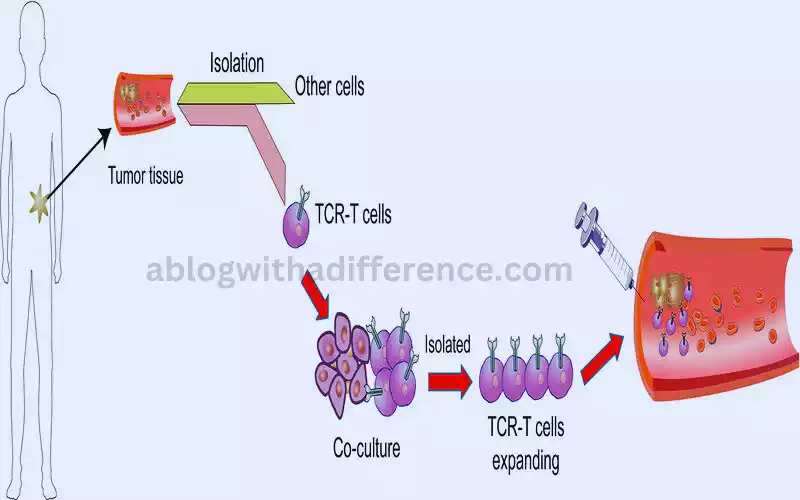
2. TCR-T Cell Therapy Manufacturing Process:
- Patient Leukapheresis: Similar to CAR-T cell therapy, the process begins with the collection of peripheral blood from the patient through leukapheresis to obtain T-cells.
- TCR Selection: T-cells expressing naturally occurring T-cell receptors (TCRs) with specificity for cancer-specific antigens are selected from the collected leukapheresis product.
- Genetic Modification: The selected T-cells undergo genetic modification to enhance their anti-cancer activity and proliferation.
- Ex Vivo Expansion: The genetically modified T-cells are cultured and allowed to expand in the laboratory, generating a sufficient number of TCR-T cells for therapeutic use.
- Quality Control: Rigorous quality control measures are implemented throughout the manufacturing process to ensure safety and efficacy.
- Cryopreservation: The final TCR-T cell product is cryopreserved for transport to the treatment site.
- Infusion: The cryopreserved TCR-T cell product is thawed and infused back into the patient through intravenous administration.
The manufacturing process for CAR-T and TCR-T cell therapies is highly specialized and performed in dedicated facilities that adhere to strict regulations and quality control standards. The complexity of the process requires close collaboration between scientists, clinicians, and manufacturing experts to ensure the production of safe and effective immunotherapies for cancer patients.
As research and technology continue to advance, efforts are focused on streamlining the manufacturing process, reducing costs, and improving accessibility to these promising treatments.
Clinical Efficacy
Immunotherapies such as CAR-T cells, TCR T cell therapy and checkpoint inhibitors have proven their clinical efficacy against various cancer types. Patients suffering refractory or advanced disease have benefitted greatly from such immunotherapies which lead to significant improvements in quality of life and survival rates.

Here are a few highlights on their clinical effectiveness:
1. CAR-T Cell Therapy:
- Acute Lymphoblastic Leukemia (ALL): CAR-T therapy has proven itself incredibly successful for treating both children and young adults with ALL who have relapsed/refractory disease. Some clinical trials have reported complete remission rates of over 80% in this population.
- Non-Hodgkin Lymphoma (NHL): CAR-T cells have proven highly successful against certain subtypes of lymphomas, particularly diffuse large B cell lymphoma and primary mediastinal B cell lymphoma; response rates ranged between 50-88%.
- Multiple Myeloma: CAR-T cell therapy has shown promise in treating multiple myeloma, particularly in patients who have failed multiple prior lines of therapy.
2. TCR-T Cell Therapy:
- Solid Tumors: TCR-T cell therapy has shown encouraging results in targeting solid tumors, including melanoma, ovarian cancer, and other malignancies expressing specific cancer-specific antigens. Clinical trials are ongoing to further assess its efficacy in various solid tumors.
- Hematologic Malignancies: TCR-T cell therapy is being explored in a range of hematologic malignancies beyond the scope of CAR-T therapy, expanding its potential application.
3. Checkpoint Inhibitors:
- Melanoma: Checkpoint inhibitors have significantly improved outcomes in advanced melanoma patients, leading to durable responses and long-term survival in some cases.
- Lung Cancer: Checkpoint inhibitors have proven their efficacy against both non-small cell lung cancer (NSCLC) and small-cell pulmonary cancer (SCLC), particularly among those expressing high levels of PD-L1.
- Renal Cell Carcinoma: Checkpoint inhibitors have demonstrated efficacy in advanced renal cell carcinoma, leading to improved response rates and survival.
- Bladder Cancer: Checkpoint inhibitors have shown promise in treating advanced or metastatic bladder cancer patients, particularly those with high PD-L1 expression.
4. Combination Therapies:
- Some patients have seen significantly better clinical results by combining immunotherapies with treatments such as chemotherapy or targeted therapy.
- Combinations of checkpoint inhibitors with other immunotherapies have demonstrated increased response rates in certain cancer types.
5. Potential for Cure:
- In some cases, immunotherapies, especially CAR-T cell therapy, have led to long-term remissions and potential cures in patients with otherwise treatment-refractory or terminal cancers.
Immunotherapies may be highly effective but not ideal for all cancer types or patients; results of treatments could depend on factors like tumor heterogeneity or an individual’s immune response to cancer treatments.
Ongoing research aims to improve patient selection, identify predictive biomarkers, and optimize treatment strategies to further enhance the clinical efficacy of immunotherapies and expand their applicability to benefit more cancer patients.
Combination Therapies
Combination therapies in cancer treatment involve using two or more different treatments in conjunction to achieve improved outcomes compared to using each therapy alone.
Combination therapies often aim to enhance treatment efficacy, overcome resistance, and minimize side effects. Combination immunotherapies such as CAR-T cells, TCR T cell therapy and checkpoint inhibitors have proven promising against different cancer types.
Some common combination strategies include:
1. Immunotherapy Combinations:
- Dual Checkpoint Inhibitors: Combining two checkpoint inhibitors that target different inhibitory immune checkpoints, such as PD-1/PD-L1 and CTLA-4, has shown enhanced anti-tumor activity in certain cancers. This approach aims to overcome immunosuppression and maximize T-cell activation against cancer cells.
- Checkpoint Inhibitors with CAR-T Cell Therapy: Administering checkpoint inhibitors alongside CAR-T cell therapy can prevent the immune system’s exhaustion and improve the persistence and function of CAR-T cells, leading to more potent anti-cancer responses.
- Combination of CAR-T and TCR-T Cell Therapies: Combining CAR-T and TCR-T cell therapies may provide broader and more potent antigen recognition, targeting both cell surface and intracellular cancer-specific antigens.
2. Immunotherapy with Traditional Treatments:
- Immunotherapy with Chemotherapy: Combining immunotherapies with chemotherapy can help enhance the immune response against cancer cells while exploiting chemotherapy’s ability to target rapidly dividing cancer cells.
- Immunotherapy with Radiation Therapy: Radiation can induce tumor cell death and release tumor antigens, potentially enhancing the immune response triggered by immunotherapies.
- Immunotherapy with Targeted Therapy: Combining immunotherapies with targeted therapies can synergize to block cancer cell growth and enhance the immune response against the tumor.
3. Immunotherapy with Personalized Vaccines:
- Personalized Cancer Vaccines: Vaccines tailored to a patient’s specific tumor antigens, known as neoantigens, can be used in combination with immunotherapies to boost the immune response against cancer cells.
- Prime-Boost Strategies: Vaccination to prime the immune system, followed by immune checkpoint inhibitors or adoptive T-cell therapy, can lead to stronger and sustained anti-tumor immune responses.
4. Sequential Therapies:
- Pre-Treatment with Checkpoint Inhibitors: Administering checkpoint inhibitors before adoptive T-cell therapies like CAR-T or TCR-T cells can prime the immune system and create a more favorable tumor microenvironment for the subsequent therapy.
- Post-Treatment with Checkpoint Inhibitors: Administering checkpoint inhibitors after CAR-T cell therapy or TCR-T cell therapy can help maintain T-cell activity and prolong treatment responses.
Combinations of immunotherapies and other treatments are an active area of research and clinical trials. Identifying the most effective and safe combination strategies for specific cancer types and patient populations is crucial for optimizing cancer treatment and improving patient outcomes.
While combination therapies show great promise, it’s essential to carefully assess potential interactions and cumulative toxicities to ensure patients receive the maximum benefit with minimal side effects.
Comparison table of CAR-T and TCR-T
Below is a comparison table highlighting the key differences between CAR-T cell therapy and TCR-T cell therapy:
| Aspect | CAR-T Cell Therapy | TCR-T Cell Therapy |
|---|---|---|
| Target Antigen | Targets cell surface antigens | Targets intracellular antigens presented by MHC |
| Recognition Mechanism | Uses chimeric antigen receptors (CARs) | Uses naturally occurring T-cell receptors (TCRs) |
| Genetic Modification | Genetically modifies T-cells to express CAR | Genetically modifies T-cells to enhance TCRs |
| Antigen Specificity | Broad antigen recognition | Narrow and specific antigen recognition |
| Antigen Range | Targets a wide range of antigens | Limited to antigens presented by MHC molecules |
| Applicability | Mostly for B-cell malignancies (e.g., ALL, NHL) | Potential for both hematologic and solid tumors |
| Approved Indications | Approved for certain ALL and NHL indications | Still in early stages of development and testing |
| Safety Profile | Associated with cytokine release syndrome (CRS) | Potential for off-target effects and cytokine release |
| Response Rate | High response rates in some B-cell malignancies | Variable response rates based on specific antigens |
| Persistence | May persist in the body for an extended period | May require additional doses to maintain efficacy |
| Manufacturing Process | CAR design and construction is a complex process | TCR selection and modification is a specialized process |
| Clinical Experience | Has more extensive clinical experience | Still limited clinical experience compared to CAR-T |
Future Directions
Researchers and clinicians alike are exploring new developments and innovations for cancer therapy, with immunotherapy promising significant breakthroughs such as CAR T cell therapy, TCR T cell therapy and checkpoint inhibitors.
Some key future directions in the field of immunotherapy include:
- Expanding Indications and Combination Therapies: As research progresses, efforts are focused on expanding the use of immunotherapies to a broader range of cancer types and stages. Combination therapies that integrate multiple immunotherapies or combine them with traditional treatments are being investigated to maximize treatment efficacy and overcome resistance.
- Targeting Solid Tumors: Immunotherapies have shown significant success in treating hematologic malignancies, but they face challenges in effectively targeting solid tumors. Future research will aim to enhance the efficacy of immunotherapies against solid tumors by targeting specific antigens or by overcoming an immunosuppressive microenvironment and increasing T-cell penetration into tumors.
- Personalized Medicine: Personalized medicine represents the future of immunotherapy. This involves tailoring treatment specifically to each patient based on his/her unique genetic makeup, tumor characteristics and immune response. Personalized cancer vaccines, neoantigen-targeted therapies, and predictive biomarkers will play key roles in guiding treatment decisions for optimal patient outcomes.
- Overcoming Resistance: Resistance to immunotherapies can occur over time. Future research should aim at identifying resistance mechanisms and devising solutions to counter them. This may involve combining immunotherapies with targeted therapies, modulating the tumor microenvironment, or employing novel approaches to boost T-cell activity.
- Improved Safety Profiles: While immunotherapies have shown significant benefits, managing immune-related adverse events (irAEs) remains crucial. Future research will seek to develop more selective and targeted therapies that minimize toxicities and improve the overall safety of immunotherapy treatments.
- Next-Generation Cell Therapies: Advances in genetic engineering and cell manipulation technologies will aid the creation of innovative cell therapies, including armored CAR T cells, dual specificity CAR T cells or allogeneic CAR T cells. These innovations aim to enhance the durability and efficacy of CAR-T cell therapy and TCR-T cell therapy.
- Access and Affordability: The widespread adoption of immunotherapies may be hindered by challenges related to cost, accessibility, and infrastructure. Future efforts will focus on making these treatments more affordable and accessible to a broader population of cancer patients worldwide.
- Predictive Biomarkers: The identification of reliable predictive biomarkers will play a crucial role in guiding patient selection, treatment response assessment, and tailoring personalized immunotherapy strategies.
- Combination with Other Therapies: Afin of improving patient outcomes, immunotherapies including radiotherapy, oncolytic virus therapy and immune modulators will be explored as potential collaborating treatments in order to enhance treatment results.
Combination with Other Therapies:
Collaboration among researchers, clinical practitioners, pharmaceutical companies and regulatory agencies will become ever more vital as immune therapy progresses further. Collaboration among these parties will accelerate clinical development while simultaneously improving cancer patients’ lives and healthcare.
With advances in immunotherapy already revolutionizing cancer treatments and our goal being personalized therapies that target specific areas more precisely being reached closer toward reality than ever before the future looks bright for this form of medicine.
Conclusion
Immunotherapies such as CAR-T and TCR T cell therapies have revolutionized cancer treatments, using our immune systems to attack cancer cells more effectively and with lower toxicity than traditional methods. These advances offer better efficacy while being safer options than their alternatives.
CAR-T therapy involves genetically engineering T cells so they produce CARs capable of recognizing specific antigens associated with cancer cells and targeting these antigens using specific antibody molecules, known as CAR chimeric receptors (CARs). CAR – T therapy has proven highly successful at treating blood cancers such as ALL or NHL.