Bone Deposition and Resorption 10 amazing difference don’t you know
Bone Deposition and Resorption are two fundamental processes that continuously occur in the human body, maintaining the balance and integrity of our skeletal system. This intricate interplay between bone formation and bone breakdown ensures that bones remain strong, healthy, and adaptable throughout our lives.
In this article we’ll delve into the fascinating world of bone metabolism, exploring its intricate mechanisms which control deposition and resorption processes as well as their significance in maintaining bone health and the factors which may impede such processes.
What is Bone Deposition?
Osteogenesis or bone formation refers to the process in which new tissues of bone are created and integrated with existing bone structures, typically through osteoblast cells that specialize in producing and releasing matrix bone tissue. This formative stage takes place both naturally and artificially through osteogenesis or bone deposition processes.
Osteoblasts produce collagen fibers as well as organic components of the bone matrix for bone deposition to occur, including calcium phosphate and other mineral deposits on collagen fibers to create hardened mineralized bone matrix structures.
When bone growth occurs osteoblasts take control by depositing calcium phosphate minerals onto collagen fibers thereby leading to mineralization processes that create hardened, mineralized structures akin to hardened steel plates or steel-reinforced walls encasing bones deposited by osteoblasts.
A bone deposition is integral for the growth, and healing of bone fractures, and maintaining strength and density of the bones. While bone deposition occurs throughout life, its importance increases during early adolescence and childhood as growth accelerates rapidly.
Bone deposition may be affected by hormonal regulation, physical stressors as well as diet that includes the recommended consumption of calcium and Vitamin D supplements.
Bone deposition and Resorption (the process by which worn-out tissues of bones are shed away), work hand in hand to preserve bone health and strength. Any imbalance could result in conditions like Osteoporosis where more bone Resorption than Bone Growth occurs causing fragile and weakening bones over time.
The Role of Osteoblasts in Bone Formation
Osteoblasts play an essential part in bone deposition or osteogenesis – also referred to as bone formation or deposition – by synthesizing and releasing elements found within bone’s matrix matrix.
Their main roles during bone development:
- Synthesis of Organic Components: Osteoblasts produce and secrete organic components, primarily collagen type I fibers, which provide the framework for bone formation. Collagen fibers form a network that gives bones their flexibility, tensile strength, and resistance to fractures. Osteoblasts also produce non-collagenous proteins like osteocalcin and osteopontin which play an integral part in bone mineralization as well as in controlling cell function in bone tissue cells.
- Mineralization of Bone Matrix: Osteoblasts facilitate the mineralization process by regulating the deposition of calcium, phosphate, and other minerals onto the collagen fibers. They release small membrane-bound vesicles called matrix vesicles that contain enzymes and proteins involved in initiating mineralization.
These vesicles help nucleate the formation of hydroxyapatite crystals, which give bones their hardness and strength. - Regulation of Osteoclast Activity: Osteoblasts indirectly play an essential role in bone resorption by controlling osteoclast function – those cells responsible for breaking down bones – through release of signaling molecules such as osteoprotegerin (OPG) and RANKL (receptor activator for nuclear factor kappa-B binding agent), Osteoblasts control development, stimulation, survival of osteoclasts. This ensures a balance between bone formation and resorption, maintaining bone health and structural integrity.
- Bone Remodeling: Osteoblasts are involved in the process of bone remodeling, which is the continuous turnover of bone tissue throughout life. Remodeling of bones involves two processes. First, damaged or worn-down bone is removed by osteoclasts; next, new bone formation occurs through osteoblasts which, together with cells like osteoclasts and their associated lining cells, work to preserve and respond to mechanical stresses within bone structures.
Osteoblast activity is determined by various variables, including growth factors, hormone signals (such as bones morphogenetic protein) mechanical load and systemic factors like vitamin D levels and calcium intake.
Imbalances in osteoblast function could result in bone disorders like osteoporosis or impairment of healing; so understanding their roles is paramount for creating treatments to stimulate new bone growth while supporting overall skeletal health.
Factors Affecting Bone Deposition
Bone deposition, the process of new bone tissue formation, is influenced by various factors. These factors include hormonal regulation, nutritional status, mechanical stress, and other systemic and local factors.
Here are the key factors that affect bone deposition:
Hormonal Regulation:
- Parathyroid Hormone (PTH): PTH stimulates bone formation indirectly by promoting the production of active vitamin D, which enhances calcium absorption from the intestines. This leads to increased calcium availability for bone mineralization.
- Calcitonin: Calcitonin helps regulate calcium and phosphate levels by inhibiting bone resorption. By reducing bone resorption, calcitonin indirectly supports bone deposition.
Nutritional Factors:
- Calcium: Sufficient calcium intake is essential for bone deposition, as calcium serves as a vital component of the bone mineral hydroxyapatite. Inadequate calcium levels can impair bone formation.
- Vitamin D: Vitamin D is crucial for calcium absorption from the intestines and the mineralization of bone.
Insufficient vitamin D levels can impair bone deposition. - Other Nutrients: Adequate amounts of magnesium, phosphorus, vitamin K and vitamin C are essential to ensure healthy bone formation.
Mechanical Stress:
- Mechanical stress and weight-bearing activities play a significant role in stimulating bone deposition. Regular physical activity and exercise, especially those that involve weight-bearing and resistance exercises, help promote bone formation. Mechanical stress triggers the activation of osteoblasts, leading to increased bone deposition in response to the demand for greater bone strength.
Hormones and Growth Factors:
Several hormones and growth factors influence bone deposition, including:
- Insulin-like Growth Factors (IGFs): IGFs promote osteoblast growth and differentiation, therefore stimulating bone formation.
- Estrogen and Testosterone: These sex hormones contribute to bone deposition during growth and development. They promote the maturation of osteoblasts and enhance bone mineralization.
- Growth Hormone: Growth hormone has an enormously beneficial impact on bone development by stimulating production of collagen as well as other protein components of bone matrix matrix proteins.
- Thyroid Hormones: Thyroid hormones are essential for normal skeletal growth and development. They regulate bone turnover and the activity of osteoblasts and osteoclasts.
Age and Hormonal Changes:
- Bone deposition is influenced by age-related changes and hormonal fluctuations. During childhood and adolescence, bone deposition is particularly active due to growth spurts and the influence of growth hormones. As people get older, hormonal fluctuations such as decreased estrogen levels in menopausal women can result in reduced bone mineralization and bone deposition.
Disease Conditions and Medications:
Certain medical conditions and medications can affect bone deposition. For example:
- Hormonal imbalances may disrupt the natural balance between bone resorption and deposition.
- Chronic inflammation and other autoimmune diseases Rheumatoid Arthritis may interfere with bone formation.
- Drugs like Glycocorticoids may impair bone development and lead to bone loss.
Understanding and addressing these factors are important for promoting optimal bone deposition and maintaining bone health throughout life.
What is Bone Resorption?
Bone resorption, or bone breakdown, occurs as part of the natural renewal of bone tissue through remodeling processes called osteoclastics.
Resorbing damaged or worn-out bone tissues allows regeneration to take place more easily while protecting skeletal health by clearing away damaged and worn out parts that hinder regeneration efforts.
Resorption plays an essential part in overall system health by eliminating worn-out components so new bone formation occurs more readily over time.

Osteoclasts attach themselves to bone surfaces and release acids and enzymes which work against mineralized bones to cause their decomposition. Enzymes like cathepsin K and acid phosphatase and K are particularly efficient at dismantling organic bone components like collagen fibers while acids dissolve crystals of hydroxyapatite which release calcium into bloodstreams.
Minerals released through degradation can be utilized for various functions in the body, including maintaining calcium balance in your system and stimulating bone remodelling and repair processes. Degradation releases growth hormones and signaling molecules which aid bone remodelling processes and repair efforts.
Bone resorption is controlled through a complex interaction among various elements, including hormones and cytokines as well as mechanical stress.
Some key contributors to bone resorption include:
- Parathyroid Hormone (PTH): Parathyroid Hormone (PTH) PTH, produced by parathyroid glands and released into bloodstream, helps maintain normal calcium levels by stimulating osteoclast activity and thus bone resorption. PTH increases bone resorption through increasing osteoclast numbers thereby leading to removal of calcium bone deposits from bone structures.
- Receptor Activator of Nuclear Factor-Kappa Ligand (RANKL): RANKL is an endocrine molecule produced by osteoblasts as well as other cells of the bone microenvironment and is essential in osteoclast development, activation and survival.
When coupled with its receptor, RANK, this chemical stimulates maturation while simultaneously encouraging osteoresorption. - Macrophage Colony-Stimulating Factor (M-CSF): Macrophage Colony Stimulating Factor (M-CSF) M-CSF is produced by osteoblasts as an additional signaling molecule to activate osteoclast differentiation and activation, working hand in hand with RANKL for maximum osteoclast activation and differentiation.
- Inflammatory Cykines: Cytokines such as interleukin-1 (IL-1) and tumor necrosis factors-alpha (TNF-alpha) have long been identified with increasing bone loss rates; chronic inflammation can exacerbate this trend, leading to excessive bone loss over time and contributing to its progression.
- Mechanical Unloading or Immobilization: Mechanical Unloading or Immobilization Over time, periods with less mechanical stress due to injury recovery or prolonged bed rest may lead to increased bone recoil. A lack of stimulation from mechanical means signals to our body’s system that this bone is no longer being utilized and causes it to increase density resulting in greater recoil and increased bone recoil.
Unbalance in bone resorption and deposition processes may contribute to osteoporosis as a bone condition.When bone resorption exceeds bone formation processes, weakening bones and increasing fracture risk – an understanding of which factors impact this process is key for formulating effective therapeutic plans to maintain and treat related illnesses.
The Role of Osteoclasts in Bone Breakdown
Osteoclasts, or bone resorbing cells, play an essential part in bone resorption – the process of breaking down worn-out or damaged bone tissues to allow new ones to form.
Osteoclasts originate as precursor cells from macrophage/monocyte families and are specially equipped to carry out bone breaking processes.
Here are their major functions in bone resorption:
- Attachment to Bone Surface: Osteoclasts attach to the bone surface at specific sites called Howship’s lacunae or resorption pits. These pits are formed by the osteoclasts themselves as they attach and create a sealed microenvironment against the bone surface.
- Acidification of Resorption Microenvironment: Osteoclasts secrete hydrogen ions (H+) through a specialized proton pump called the H+-ATPase. This leads to acidification of the resorption microenvironment, creating an acidic pH that aids in the breakdown of mineralized bone tissue.
- Secretion of Enzymes and Acids: Osteoclasts release various enzymes and acids into the resorption microenvironment. The enzymes, including acid phosphatase and cathepsin K, degrade the organic components of the bone matrix, particularly collagen fibers. Cathepsin K is particularly important for the degradation of collagen, which is a major component of bone tissue.
- Resorption of Mineralized Bone: Osteoclasts create a tightly sealed compartment, called the resorption lacuna, against the bone surface. Within this compartment, the acidic environment, along with the action of enzymes, facilitates the dissolution of the mineralized bone matrix. The released calcium, phosphate, and other minerals are then absorbed into the bloodstream.
- Regulation by Signaling Pathways: The activity of osteoclasts is tightly regulated by various signaling pathways. The receptor activator of nuclear factor-kappa B ligand (RANKL) is a key signaling molecule that stimulates osteoclast formation, activation, and survival. Osteoprotegerin (OPG) acts as a decoy receptor for RANKL and helps to inhibit osteoclast activity, thereby regulating bone resorption.
- Interaction with Osteoblasts: Osteoclasts interact with osteoblasts – cells responsible for bone formation – through coupling. Osteoblasts release factors like RANKL which enhance osteoclast development and activity, creating an even balance in remodelling processes which helps ensure healthy bones.
Unbalanced osteoclast activity may contribute to various bone-related conditions, including osteoporosis (which occurs when bone loss becomes excessive). Achieve bone health through controlled osteoclast activity by understanding their roles and controlling osteoclast activity as effectively. Understanding their function allows treatment designs that may prevent excessive bone resorption while protecting bone integrity.
Factors Affecting Bone Resorption
Resorbing bone tissue involves breaking it down through various mechanisms; such influences may impact osteoclast activity responsible for bone resorption.
Here are a few elements which influence this process of bone resorption:
1. Hormonal Regulation:
- Parathyroid Hormone (PTH): PTH stimulates bone resorption indirectly by promoting the production of active vitamin D, which enhances calcium absorption from the intestines. Increased PTH levels result in increased bone resorption.
- Calcitonin: Calcitonin is an antiresorption hormone which reduces osteoclast activity while simultaneously maintaining calcium levels within your system.
2. Inflammatory Cytokines:
- Inflammatory cytokines such as interleukin-1 (IL-1) and tumor necrosis factor alpha (TNF-alpha), have long been shown to accelerate bone loss. They can be produced as the result of illness, autoimmune conditions or inflammation-related issues and lead to further loss.
3. Mechanical Unloading or Immobilization:
- Lack of mechanical stress on bones, such as in prolonged bed rest or immobilization due to injury, can result in increased bone resorption. Mechanical loading and weight-bearing activities stimulate bone formation, so the absence of such activities can lead to an imbalance favoring bone resorption.
4. Aging and Hormonal Changes:
- As individuals age, hormonal changes occur, leading to alterations in bone turnover.
As menopausal women experience lower estrogen levels, bone resorption increases. Men are similarly subject to hormonal fluctuations which cause their bone mass to diminish over time due to age-related decline.
5. Disease Conditions and Medications:
- Certain diseases and medications can increase bone resorption. Osteoporosis and hyperparathyroidism and hyperthyroidism as well as cancerous tumors as well as certain drugs which alter bone metabolism are examples.
6. Calcium and Vitamin D Imbalances:
- Lacking sufficient calcium and vitamin D could disrupt the delicate balance between bone resorption and deposition. Low calcium levels can trigger increased PTH secretion, leading to increased bone resorption. Vitamin D deficiency can impair calcium absorption and utilization, further compromising bone health.
7. Genetic Factors:
- Genetic factors can influence an individual’s predisposition to increased bone resorption. Certain genetic variants may alter osteoclast activity and alter bone turnover rates, leading to an uneven rate.
Resorbing bone is an integral component of bone remodelling and should occur naturally over time – although excessive or prolonged osteoporosis without sufficient deposition of new bones could result in its loss, increasing your risk of breaking.
Being aware of these risks and adopting healthy practices such as healthy nutrition and regular physical activity is vital in order to preserve and protect bone health as well as lower chances of bone-related diseases such as osteoporosis.
Comparison table of Bone Deposition and Resorption
Here’s a comparison table highlighting the key differences between bone deposition and bone resorption:
| Aspect | Bone Deposition | Bone Resorption |
|---|---|---|
| Definition | The process of adding new bone tissue to the existing bone structure. | The process of breaking down and removing old or damaged bone tissue. |
| Cell involved | Osteoblasts | Osteoclasts |
| Function | Builds and strengthens bones. | Removes old or damaged bone tissue. |
| Process | Synthesis and secretion of collagen fibers and other organic components of the bone matrix. Mineralization of the bone matrix. | Attachment to bone surface, secretion of enzymes and acids, and breakdown of mineralized bone matrix. |
| Factors influencing process | Hormonal regulation, nutritional factors, mechanical stress. | Hormonal regulation, inflammatory cytokines, mechanical unloading, aging. |
| Role in bone remodeling | Adds new bone tissue during growth, repair, and maintenance of bone density. | Removes old or damaged bone tissue, facilitates bone reshaping, and maintains calcium homeostasis. |
| Importance for bone health | Essential for maintaining bone strength, density, and integrity. | Necessary for maintaining balanced bone remodeling, calcium regulation, and adaptation to mechanical stress. |
| Imbalance consequences | Excessive bone deposition can lead to increased bone density disorders. | Excessive bone resorption can lead to decreased bone density disorders. |
| Examples of related disorders | Osteopetrosis (excessive bone deposition) | Osteoporosis (excessive bone resorption) |
| Cell-cell communication | Coupled with osteoclasts through signaling molecules like RANKL and OPG. | Coupled with osteoblasts through signaling molecules like RANKL and OPG. |
Dynamic Balance between Bone Deposition and Resorption
The skeletal system undergoes continuous remodeling throughout life, which involves a dynamic balance between bone deposition and bone resorption.
This process, known as bone remodeling, ensures the maintenance of bone strength, repair of microdamage, and adaptation to mechanical stresses. The interplay between bone deposition and resorption is essential for skeletal health and integrity.
Resorption and deposition of bone are carefully orchestrated through complex molecular and cell-based mechanisms. Osteoblasts play an integral part in bone deposition while osteoclasts aid with its removal.
Here’s an overview of the dynamic balance between these two processes:
- Bone Deposition:
-
- Osteoblasts: These specialized bone-forming cells synthesize and secrete collagen fibers and other organic components of the bone matrix. They also promote the mineralization of the bone matrix by depositing calcium and other minerals onto the collagen framework.
- Factors promoting bone deposition: Hormones such as parathyroid hormone (PTH) and calcitonin as well as growth factors like insulin-like growth factors (IGF) play an essential role in stimulating osteoblast activity, as do proper amounts of calcium, phosphate, and vitamin D for bone formation.
- Functions of bone deposition: Bone deposition helps repair microdamage, strengthen bones in response to mechanical stress, and maintain bone density during growth and development.
- Bone Resorption:
-
- Osteoclasts: These specialized cells derived from monocyte/macrophage lineage are responsible for bone resorption. Osteoclasts attach to the bone surface and secrete enzymes and acids that degrade the mineralized bone matrix.
- Factors promoting bone resorption: Hormones such as parathyroid hormone (PTH), nucleotide receptor activator nuclear factor-kappa B ligand (RANKL), and proinflammatory cytokines may stimulate osteoclast activity and encourage bone resorption, while conditions that produce acidosis, such as elevated amounts of certain cytokines may accelerate bone loss further.
- Functions of bone resorption: Bone resorption allows for the removal of old or damaged bone tissue, facilitates calcium and mineral homeostasis, and enables bone reshaping and adaptation to mechanical stresses.
- Coupling of Bone Deposition and Resorption: Bone remodeling involves the coordinated action of osteoblasts and osteoclasts in a process known as coupling. Osteoblasts and osteoclasts communicate through signaling molecules, including RANKL and osteoprotegerin (OPG). Osteoblasts secrete RANKL, which binds to its receptor on osteoclasts and promotes their activation and resorption. OPG acts as a decoy receptor, binding to RANKL and inhibiting osteoclast activity. This coupling ensures that bone resorption is followed by bone deposition at the same site, maintaining the integrity and strength of the bone.
Instabilities in bone remodeling could contribute to bone-related disorders like osteoporosis.
When bone deposition exceeds bone resorption, density drops significantly and fracture risk rises, ultimately increasing fracture risks and leading to decreased density overall.
Understanding the dynamic balance between bone deposition and resorption is crucial for diagnosing and managing bone-related conditions and developing interventions to optimize bone health.
Age-Related Changes in Bone Deposition and Resorption
As people get older, many changes occur during bone deposition and resorption that lead to changes related to aging in bone health. These changes can impact bone density, strength, and overall skeletal integrity.
Here are some age-related changes in bone deposition and resorption:
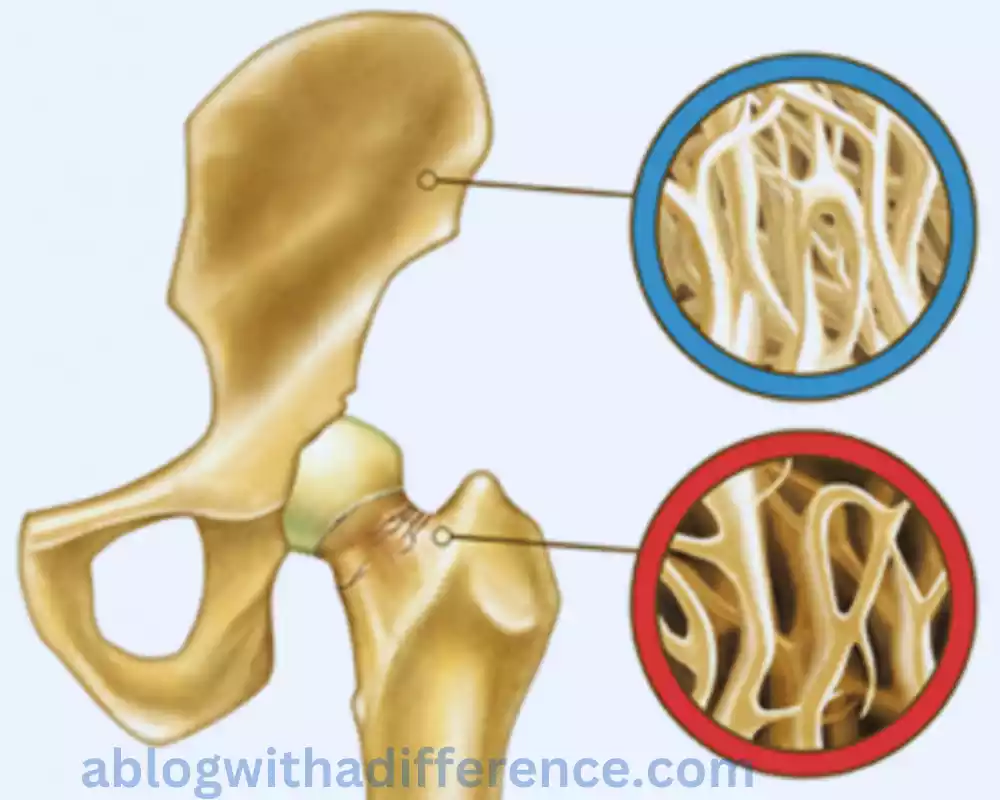
- Decreased Bone Formation: As we get older, it becomes apparent that osteoblasts (cells responsible for bone deposition) gradually slow their activity and start decomposing bone more slowly than before. Osteoblasts become less efficient in synthesizing and secreting collagen fibers and other organic components of the bone matrix. This reduced bone formation contributes to age-related bone loss.
- Imbalance Between Bone Formation and Resorption: As individuals age, there is often a shift towards increased bone resorption compared to bone formation. Osteoclast activity, responsible for bone resorption, may become more dominant or less effectively balanced by osteoblast activity.
- This imbalance results in a gradual loss of bone mass and density.
- Changes in Hormonal Regulation: Hormonal changes that occur with age can influence bone remodeling. Women experiencing postmenopausal transition experience an unexpected decrease in estrogen levels after menopause; this drop can increase osteoporosis and bone loss. Male counterparts likewise find their testosterone levels decline affecting bone health negatively.
- Alterations in Calcium and Vitamin D Metabolism: Changes in calcium and vitamin D metabolism with age Effects bone deposition/resorption When combined, changes to calcium and vitamin D metabolism with age could significantly impact both processes.
- The efficiency of intestinal calcium absorption may decrease, leading to reduced calcium availability for bone mineralization. Inadequate vitamin D levels can impair calcium absorption and utilization, further compromising bone health.
- Decreased Response to Mechanical Stress: Aging bones may become less responsive to mechanical stress, resulting in reduced bone formation. Older individuals may experience decreased physical activity, which can further contribute to bone loss due to reduced mechanical loading on the bones.
- Increased Bone Resorption Markers: Aging has been associated with increases in biochemical markers of bone resorption such as tartrate-resistant acid phosphatase (TRAP) and C-terminal Telopeptide from type I collagen (CTX), both suggesting rapid rates of bone degradation and the consequent resorption. These indicators of osteoclast loss indicate an increasing rate of degradation and bone loss, signaling to medical professionals the need to intervene to preserve bone health and its future generations.
- Structural Changes: Age-related structural alterations such as increased porosity or loss of trabecular connections could further weaken bones, increasing their likelihood of breaking.
Changes caused by age are a natural part of getting older; however certain triggers such as poor diet, sedentary lifestyles, and medical problems could increase bone loss in older people. Exercise routine, a healthy diet rich in calcium and vitamin D, and medical intervention could all play a part in combatting bone resorption/deposition and thus potentially decreasing your chances of fractures.
The Impact of Nutrition on Bone Health
Nutrition plays a pivotal role in maintaining optimal bone health throughout your lifetime. A proper intake of nutrients is required for proper bone development growth maintenance and repair –
Here are the key nutrients with major impacts on bone wellness:
- Calcium: Calcium is one of the main constituents of bone, providing its strength and rigidity. A sufficient supply of calcium-rich food such as dairy products or leafy green vegetables as well as dairy alternatives with plant-based milk fortification or calcium supplements should help ensure proper bone mineralization. A diet rich in this element should ensure optimal mineralization. A proper supplementation regime could be implemented if required.
- Vitamin D: Essential to calcium absorption in the intestinal tract and bone mineralization, vitamin D can also play an integral part in making sure food sources such as fish oils, fortified dairy products, and supplements provide enough Vitamin D. Sunlight is our main source for Vitamin D; other sources may include fortified dairy products like cottage cheese as well as supplements.
- Phosphorus: Phosphorus is an integral mineral component of bone that works alongside calcium to create crystals of hydroxyapatite that help strengthen it. Fish, meat, and dairy products as well as poultry provide great sources of phosphorus; other sources including nuts legumes, or grains are great options as well.
- Magnesium: Magnesium plays an essential role in bone formation and metabolism; its lack can impede enzyme functions responsible for this process. Good sources of magnesium include whole grains, seeds, nuts legumes leafy green veggies plus dark chocolate as good sources.
- Vitamin K: Broccoli, green leafy vegetables, Brussels sprouts, and fermented foods all make great sources of Vitamin K for activating proteins involved with bone mineralization. It may even play a part in stimulating bone healing during recovery after bone surgery!
- Protein: Protein plays an integral part in bone matrix formation. Its presence aids growth, repair, and reconstruction processes as well as maintaining health in general. A proper protein intake from both plant and animal sources is necessary for maintaining bone health.
- Omega-3 Fatty Acids: Omega-3 Fatty Acids provide anti-inflammatory benefits and may assist with bone density restoration by decreasing bone loss and increasing bone mass. Mackerel, salmon, flaxseeds with walnuts, or chia seeds are excellent sources of these essential fatty acids.
- Other Micronutrients: Zinc copper zinc and vitamin C help support bone health in multiple ways by aiding various aspects of metabolism as well as collagen production. Vitamin B12 and A also play important roles.
The essence of bone health involves maintaining an appropriate and diverse diet packed with the vitamins and nutrients essential for its maintenance.
Exercising regularly, foregoing alcohol or tobacco smoking, and maintaining weight in an ideal manner are also helpful ways of supporting optimal bone health overall.
Speaking to an expert healthcare practitioner or certified dietitian can offer customized advice about meeting nutritional requirements to achieve maximum bone health benefits.
Common Disorders Related to Imbalance in Bone Metabolism
There are various bone diseases caused by problems in their metabolism that result in bone loss or resorption, leading to impaired health, decreased density, and an increased likelihood of breaking.
Here are a few instances:
- Osteoporosis: Osteoporosis is a condition characterized by reduced bone mass and degraded tissue that ultimately results in greater fragility, increasing fracture risk. Osteoporosis occurs because bone loss outpaces formation rates causing density levels to decrease over time resulting in osteoporosis becoming the more prominent form among postmenopausal women due to reduced estrogen levels following menopause – it’s the leading form of this form.
- Osteopenia: Osteopenia refers to bone mineral density levels below normal but aren’t yet at osteoporosis-level, and may indicate potential future osteoporosis cases. Osteopenia can serve as an early warning sign and could indicate osteoporosis before its time arrives.
- Paget’s Disease of Bone: Paget’s disease of bone is a chronic illness that is the result of abnormalities in bone remodeling, including excessive bone loss through osteoclasts followed by disorganized osteoblastic growth which leaves affected bones weak, enlarged, vulnerable, and likely to fractures.
- Paget’s can affect one or multiple bones throughout a person’s pelvis, skull spine as well and long bones – but is usually found affecting the pelvis skull spine as well as long bones.
- Osteomalacia: Osteomalacia refers to bones becoming soft due to insufficient mineralization caused by vitamin D deficiency or impairment, often as the result of vitamin D metabolism impairment or inadequate supplementation.
- Over time this could result in weak bones which cause pain for muscles as well as increased fracture risk.
- Rickets: Rickets is an uncommon condition affecting children that results from insufficient mineralization of bones during bone growth, often as the result of vitamin D deficiencies or reduced vitamin D metabolism.
- The outcome can include malformed growth patterns, muscle weakness, and increased fracture risks – symptoms are easily identified through its name alone!
- Hyperparathyroidism: This condition results from the overproduction of parathyroid (PTH) hormone from the glands of parathyroid, leading to excessive amounts of bone-resorbing PTH levels that could result in osteoporosis, bone loss, and increased fracture risks. A rise in PTH levels could cause more bone resorption leading to osteoporosis as well as higher risks of fracture.
- Renal Osteodystrophy: Cause and Consequences The term “renal” denotes osteodystrophy as being caused by kidney diseases (CKD). Changes to hormone and mineral balance caused by kidney diseases may alter bone turnover resulting from reduced formation and increased loss. This condition often results in bone pain, fractures or deformities, and even bone pain syndromes.
Identification and treatment of bone disorders must take into account both complications as well as improvements to overall bone health, including prevention measures such as lifestyle modifications, nutrition with calcium/Vitamin D supplements, medications, or hormonal replacement therapy as needed.
It’s advisable to seek guidance from medical specialists such as endocrinologists/rheumatologists/orthopedists/orthopedic specialists when diagnosing and treating these diseases for proper diagnosis and management.
Conclusion
Resorption and deposition are integral processes in bone remodeling and maintaining skeletal health. Deposition occurs via osteoblasts which produce and release collagen fibers for mineralization while bone resorption occurs via osteoclasts which break down and remove damaged or old bone tissue.
Balance between bone deposition and resorption is vital in maintaining overall bone health, especially the long-term health of our bones.